 September is National Suicide Prevention Month and along with continuing to inform people about warning signs, Texas Children’s has recently elevated our prevention tactics with the use of the Columbia Suicide Screening Rating Scale (C-SSRS).
September is National Suicide Prevention Month and along with continuing to inform people about warning signs, Texas Children’s has recently elevated our prevention tactics with the use of the Columbia Suicide Screening Rating Scale (C-SSRS).
“Texas Children’s Hospital recognizes that our team, our system has an essential role to play in helping young people and their families who may be struggling with mental health problems and suicidal thoughts or actions,” said the Chief of Psychiatry at Texas Children’s Hospital, Dr. Laurel Williams. “Over the past 18 months our Psychiatry, Social Work, Psychology, Nursing and Pediatrician partners have been improving our assessment and care for these young people.”
According to the Columbia Lighthouse Project, C-SSRS supports suicide risk assessment through a series of simple, plain-language questions. The answers help users identify whether someone is at risk for suicide, assess the severity and immediacy of that risk, and gauge the level of support that the person needs.
Texas Children’s is currently using the C-SSRS in all three emergency rooms for all youth over the age of 11 since March 2018, and to date we have screened more than 1,700 adolescents. Individuals who screen positive are given specific treatment plans based on the level of severity, including either further assessments by our psychiatry team or our partners, Mental Health Solutions. Mental Health Solutions is an outside team of social workers who will come to our hospital emergency rooms to assist parents. Their health care teams also locate appropriate locations for inpatient psychiatric care within Houston and surrounding counties for youth needing such specialty services.
“Additionally, the inpatient teams have undergone increased training for nurses and patient sitters in order to better address mental health needs for patients with either suicidal thoughts/actions or aggressive behaviors,” Dr. Williams said. “A safety sweep checklist was developed and is employed for any young person identified as having suicidal thoughts or actions to improve the care environment for them while admitted to our care.”
Suicide is the second leading cause of death in the United States among adolescents between the ages of 15 and 24. This is more than cancer, diabetes, cardiac and neurologic diseases and yet there is still a stigma attached to suicide. Over 450,000 emergency rooms visits annually are secondary to individuals who have self-inflicted injuries.
“This screening process has allowed our team at Texas Children’s Hospital to act on the information received to intervene prior to a suicide attempt,” Williams said. “A treatment plan is also designed to avert harm and improve the patient’s mental health.”
Future plans for C-SSRS include screening other localities within our system such as specialty and general pediatric clinics in conjunction with depression screening.
Suicide is preventable and overall, mental health disorders do have effective treatments. We encourage our entire team to fight against the stigma. For those who might be experiencing suicidal thoughts we encourage everyone to consider the following resources:
- Emergency or urgent needs – 1-800 273-TALK (8255)
- Texas Children’s Hospital’s Psychiatry Clinic, For outpatient assessments and treatment – 832-822-3750
- Texas Children’s Hospital Employee Assistance Program – 832-824-3327
Click here to learn more about suicide prevention. Click here to become more involved in suicide prevention awareness.



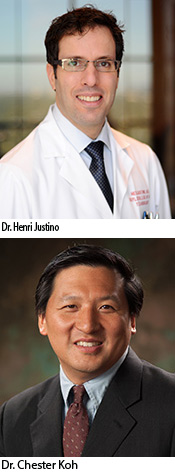 The Southwest Pediatric Device Consortium (SWPDC), anchored at Texas Children’s Hospital and Baylor College of Medicine, recently received a prestigious P50 grant from the U.S. Food and Drug Administration. The five-year, $6.75 million grant will begin on September 1 and will allow SWPDC to leverage ongoing activities to expand and accelerate the development of much-needed pediatric medical devices. The five principal investigators include Drs. Chester Koh and Henri Justino of Texas Children’s and Baylor, Dr. Balakrishna Haridas of Texas A&M University, Dr. Maria Oden of Rice University, and Dr. Michael Heffernan of Fannin Innovation Studio.
The Southwest Pediatric Device Consortium (SWPDC), anchored at Texas Children’s Hospital and Baylor College of Medicine, recently received a prestigious P50 grant from the U.S. Food and Drug Administration. The five-year, $6.75 million grant will begin on September 1 and will allow SWPDC to leverage ongoing activities to expand and accelerate the development of much-needed pediatric medical devices. The five principal investigators include Drs. Chester Koh and Henri Justino of Texas Children’s and Baylor, Dr. Balakrishna Haridas of Texas A&M University, Dr. Maria Oden of Rice University, and Dr. Michael Heffernan of Fannin Innovation Studio.



 Texas Children’s Cancer and Hematology Centers, Baylor College of Medicine International Pediatric AIDS Initiative at Texas Children’s Hospital (BIPAI) and several global partners recently celebrated the graduation of the first class of the East African Pediatric Hematology and Oncology Fellowship Program at Makerere University College of Health Sciences.
Texas Children’s Cancer and Hematology Centers, Baylor College of Medicine International Pediatric AIDS Initiative at Texas Children’s Hospital (BIPAI) and several global partners recently celebrated the graduation of the first class of the East African Pediatric Hematology and Oncology Fellowship Program at Makerere University College of Health Sciences.