Due to a high demand for our expert maternal fetal medicine services and our goal to keep access open to all patients who need our care, Texas Children’s Pavilion for Women has expanded its Maternal Fetal Center.
Located on the fourth floor of the Pavilion for Women, the center serves high-risk obstetrical patients and also bridges access to our pediatric subspecialists for our youngest patients through our Fetal Center program.
“The unit is designed so that the majority of services and partners needed to participate in a pregnancy come to us,” said Assistant Director of Ambulatory Clinical Practices for Women’s Services Aimee Jackson. “We pride ourselves on being a one-stop shop for our patients and families, providing timely, comprehensive, coordinated care in one place.”
Since opening its doors in 2012, the center has seen an 11 percent increase in patient visits. Last year, the center saw 36,000 patient visits and is expected to see 40,000 this year.
To continue to provide this growing patient population, construction on the Maternal Fetal Center began in September and was completed seven months ago at the end of April. The expansion added the following:
- Three exam rooms bringing the total number of exam rooms in the center to nine. One of the exam rooms was built specifically for fetal intervention total care patients. These patients now can have their ultrasound, clinic visit and antenatal testing visit all in one location at the center. Historically, these patients had to schedule several different appointments in several different places to get these services.
- Two ultrasound rooms, bringing the total number to 11. One of the new can be used for clinical imaging as well as imaging research and educational training.
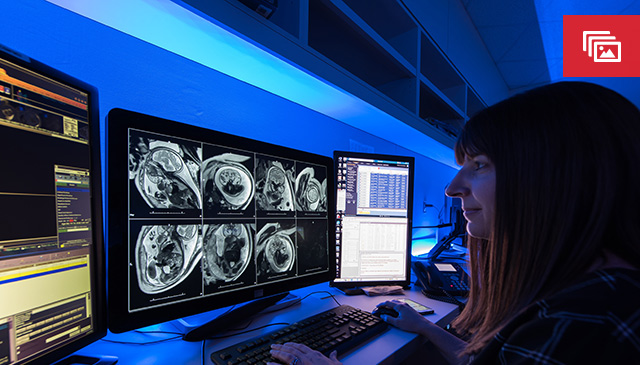
- A second conference room equipped with advanced imaging display capabilities. The room will be used for team and family meetings as well as patient classes.
- A large multi-person office space to accommodate the center’s expanded nursing and business support teams.
- In addition, the center’s two existing reading rooms for radiology and cardiology were renovated, expanded and optimized.
“We have needed this for a long time,” said Dr. Manisha Gandhi, the center’s medical director. “Most of our patients hoped they would never need our services, therefore we want to make their stay with us as comfortable as possible. This expansion will help us do that at an even higher level than we are now.”
Dr. Wesley Lee, chief of women and fetal imaging, agreed and said the center’s care team is committed to treating, respecting, and embracing patients with a spirit of hope and perseverance.
“Having the right space to carry out this type of care is key,” Lee said. “We are thrilled to have this extra space and to be able to use it to better serve our patients.”
Texas Children’s Pavilion for Women also is expanding its maternal fetal services at its community locations in the Greater Houston and beyond. Here are some of the latest developments:
Baytown: In April, the Baytown Maternal Fetal Medicine Clinic moved to a larger space at Houston Methodist Baytown Hospital. The clinic – which offers maternal fetal consulting and ultrasound, as well as nutrition, genetic and psychiatric counseling – opened in 2016 for just one day a week. The number of patients coming to the clinic steadily increased, prompting leadership in 2018 to keep the clinic’s doors open five days a week. Today, the clinic’s team sees 10 to 15 patients a day. The majority of those patients, 70 percent, are seen by clinicians via telemedicine. The remaining 30 percent are seen by in-house medical staff.
Medical Center: In June, the Maternal Fetal Medicine Clinic in Houston Methodist Hospital’s Smith Tower in the Medical Center expanded from two ultrasound rooms to three and one non-stress test chair to two. As a result, the clinic can see more patients for Maternal Fetal Medicine services as well as nutrition and genetic counseling.
Lufkin: In November, a maternal fetal medicine clinic is slated to open at CHI St. Luke’s Health Memorial-Lufkin. Ultrasound and maternal fetal consults will be offered.
“Our aim with these community clinics is to provide excellent patient care closer to where some of our patients live,” said Jennifer Dalton, patient care manager for the Pavilion for Women Community Clinics. “We don’t want them to have to drive to the Medical Center unless they absolutely have to.”
Akachi Phillips, manager for the Pavilion for Women Community Clinics, said she knows a patient from Louisiana who drove weekly to the Medical Center for her visits during one of her pregnancies. During a subsequent pregnancy, she was able to have her ultrasounds in Baytown, which cut down her travel time and enhanced her overall experience.
“It means a lot to the patients to have a clinic nearby,” Phillips said.
For more information about the Maternal Fetal Center, click here.











