Texas Children’s has achieved HIMSS Stage 7 designation for Inpatient and Ambulatory across the system, which demonstrates the organization’s successful implementation of health care information technology to address quality initiatives and improve the delivery of patient care, efficiency and safety. In 2019, only 7 percent of hospitals in the U.S. achieved Stage 7 designation.
“Our hospital is among a small, elite group of health care organizations in the nation that have been awarded Stage 7 designation for inpatient and outpatient facilities,” said Myra Davis, senior vice president of Information Services. “This collaborative milestone is a culmination of nearly a decade of implemented technological solutions and data gathering to advance patient outcomes and further differentiate Texas Children’s from other hospitals that provide care for children and women.”
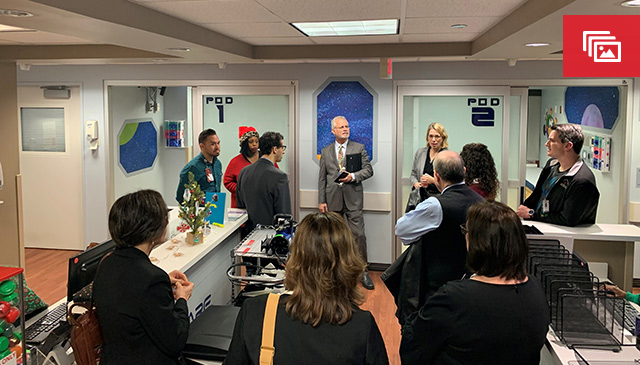
Reviewers from HIMSS Analytics visited Texas Children’s Medical Center Campus on December 16 and 17 to validate the organization’s achievement of Stage 7 in our inpatient and outpatient facilities, including Texas Children’s Pediatrics on Kirby Drive. Staff answered questions about the hospital’s use of technology to support patient care including processes for clinical information documentation, tools for quality metrics and analytics, and the handling of paper documents.
“It was wonderful to hear reviewers acknowledge our Quality and IS collaboration as being ‘best in class’, among other notable mentions,” said Texas Children’s Chief Medical Information Officer Dr. Carla Giannoni. This has been a goal that we, as an organization, have been actively focused on achieving.
HIMSS reviewers noted several key IS achievements that contributed to our Stage 7 designation:
- Optimizing clinical workflows – This has improved the quality of care across the system whether in the emergency center or at a primary care practice. Epic’s electronic mobile application suite allows providers to e-prescribe medications and improves the safe and secure transmission for patient health information among providers.
- System integrations – Integration of the PACS link in Epic for imaging review and lab results has provided our providers with a holistic view to determine a more personalized plan of care. A system integration that was implemented is MyDining, a new room service feature that offers healthier menu options for patients during their hospital stay.
- Electronic health record (EHR) enhancements – Examples of enhancing the EHR include decision support in the form of Best Practice Alerts that automatically notify staff of certain conditions such as the risk of Sepsis or the need for an influenza immunization.
“The maturity of health information technology and data analysis are key to advancing outcomes and experience for our patients and providers,” said Julie McGuire, director of Enterprise Systems for Information Services. “We are so grateful to have completed this last step in our Stage 7 journey. We were able to achieve this designation through the collaborative support from our dedicated partners.”
The tireless leadership of the planning team members from several departments that contributed to Texas Children’s obtaining Stage 7 designation included Quality, Radiology, Pharmacy, Texas Children’s Pediatrics/Texas Children’s Urgent Care, Health Information Management, Nursing Clinical Informatics, Chief Medical Information Officer and Associate Medical Information Officers, Mission Control, subspecialty services (Pediatrics, Surgery and Women’s Services), Pathology, Emergency Management and all employees and staff who hosted the site visits in their respective areas.
“Our goal is to optimize the digital tools that surround the providers so we can radically improve our performance and deliver better care,” said Texas Children’s Chief Quality Officer Dr. Eric Williams. “We are proud of the Stage 7 designation, but we are more proud of how our digital transformation has improved patient care.”