Texas Children’s marked the beginning of an exciting chapter in its history Thursday when President and CEO Mark A. Wallace joined other organization leaders in celebrating the opening of Texas Children’s Urgent Care Westgate – the first Texas Children’s location in Austin.
“It’s great to be in Austin,” Wallace said during a private ribbon cutting ceremony for clinical staff and Texas Children’s leaders. “We can’t wait to serve the children, women and families of the greater Austin area.”
View event photos below.
Texas Children’s leaders announced in June their plan to open a pediatric-focused urgent care in Austin, with the goal of supplementing the great health care options already available to the community and improve access to care, at nights and on weekends, in a convenient location. Texas Children’s Urgent Care Westgate at 4477 South Lamar Blvd. is modeled after other Texas Children’s urgent care facilities, all of which are located in the Greater Houston area and offer high-quality, efficient and affordable pediatric care at a convenient location.
Open Monday through Friday, 4:30 p.m. to 11 p.m. and Saturday and Sunday, noon to 8 p.m., Texas Children’s Urgent Care Westgate is staffed by board certified pediatricians who diagnose and treat a wide variety of ailments, illnesses and conditions, including: asthma, strep throat, fever, minor burns, influenza, ear infections, allergic reactions and more. Procedures to be provided include: antibiotic injections, breathing treatments, fracture care and splinting, IV (intravenous) fluids, lab services, laceration repair and X-rays onsite.
“As we all know, children are not simply tiny adults; their medical care, as well as the tools and equipment used, should be designed specifically to meet their needs,” said Dr. Lisa Gaw, lead physician at Westgate. “This is why it is important children are seen and treated by the experts trained to care for them. We are proud to have created a place local pediatricians and caregivers can feel confident sending their children knowing they will be well cared for by experts specially trained in treating kids.”
Texas Children’s opened its first urgent care facility in 2014 and has since seen tremendous success in getting pediatric patients where they need to be to receive the proper treatment for their illness or injury, decreasing the number of low-acuity cases at Texas Children’s emergency rooms.
In addition to opening Texas Children’s Urgent Care Westgate, Texas Children’s plans to open additional pediatric urgent care clinics, primary care pediatric practices, pediatric specialty care locations and maternal-fetal medicine practices across Austin over the next five years.
“This opening is the first step in a thoughtful plan Texas Children’s has in place to bring pediatric-focused care to Austin in a way that will help us serve the state of Texas even more successfully,” said Executive Vice President Michelle Riley-Brown, who leads Texas Children’s community and outpatient strategy. “We aspire to collaborate with the many established pediatric providers in the region to help support the growing Austin market, and see our growth in the area as an extension of our mission to ensure women and children have access to exceptional health care close to home.”
To learn more about Texas Children’s efforts in Austin, click here, and to find out more about Texas Children’s Urgent Care, click here.





















 Less than two months after being separated from her sister Hope in a seven-hour surgery at Texas Children’s Hospital, Anna Grace Richards got to go home.
Less than two months after being separated from her sister Hope in a seven-hour surgery at Texas Children’s Hospital, Anna Grace Richards got to go home.




 Recently, Texas Children’s executives and employees welcomed Judy Faulkner, CEO and founder of Epic Systems. Faulkner walked the group through a timeline of successes and innovations that have resulted from Texas Children’s 10-year partnership with Epic.
Recently, Texas Children’s executives and employees welcomed Judy Faulkner, CEO and founder of Epic Systems. Faulkner walked the group through a timeline of successes and innovations that have resulted from Texas Children’s 10-year partnership with Epic.



















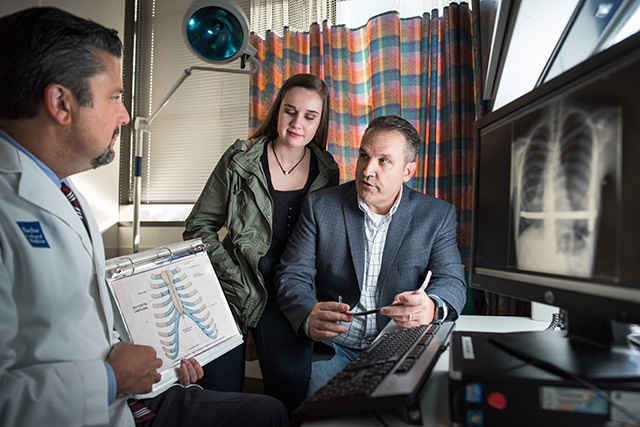 It’s not every day that physicians at Texas Children’s get the opportunity to treat a child and their parent, but that’s exactly what happened when Caitlin King became a patient of Texas Children’s Pectus Program.
It’s not every day that physicians at Texas Children’s get the opportunity to treat a child and their parent, but that’s exactly what happened when Caitlin King became a patient of Texas Children’s Pectus Program.






















