 More than 300 members of the Texas Children’s Hospital Department of Surgery attended the eighth annual Edmond T. Gonzales, Jr., Surgical Research Day on May 19. The event provided a forum for researchers across the department to showcase their work.
More than 300 members of the Texas Children’s Hospital Department of Surgery attended the eighth annual Edmond T. Gonzales, Jr., Surgical Research Day on May 19. The event provided a forum for researchers across the department to showcase their work.
“As the research enterprise within the Department of Surgery grows, this day, where we highlight the research being conducted in the department, is more important than ever,” said Dr. Charles D. Fraser, Jr., surgeon-in-chief at Texas Children’s Hospital. “The new research discoveries coming from academic surgeons and scientists at Texas Children’s Hospital are changing the future of health care.”
This year 159 abstracts were submitted for review. Eleven of these abstracts were chosen for oral presentations on Surgical Research Day and 130 were accepted for poster presentations. This year eight students vied for the Best Presentation award and three faculty members were chosen to present their research.
The 2016 keynote speaker was Dr. Michael Longaker, the Deane P. and Louise Mitchell Professor and Vice Chair of the Department of Surgery at the Stanford University School of Medicine and Lucile Salter and Packard Children’s Hospital. He is a pediatric plastic surgeon who also directs Stanford Medical School’s Program in Regenerative Medicine and Children’s Surgical Research, and co-directs the Institute of Stem Cell Biology and Regenerative Medicine.
Laura Laux Higgins, director of special projects in the Department of Surgery at Texas Children’s Hospital, gave an ethics presentation on ethical violations in research. Higgins worked at leading legal firms as a litigator and spent several years at a top management consulting firm before joining Texas Children’s.
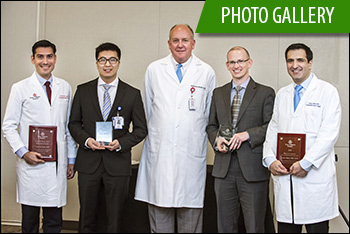
Awards presented at the event were the Samuel Stal Research Award for outstanding research by a resident or fellow, the Research Mentor Award, and Best Oral Presentation and Best Poster Presentation.
- The Samuel Stal Research Award was presented to Dr. Luis De Leon, a post-doctoral research fellow in Congenital Heart Surgery. The award is named after Dr. Samuel Stal, former chief of Plastic Surgery at Texas Children’s.
- Congenital Heart Surgeon Dr. Carlos Mery was honored with the Research Mentor Award. The award is given on an annual basis to honor a Department of Surgery faculty member who serves as a research mentor through career development, professional guidance or cultivation of research interests.
- Best Oral Presentation award was given to Dr. James Fisher who is in the first year of his fetal surgery fellowship. He presented his work on the Development and Validation of a Fetal 3-D Surgical Simulator: Implications for Minimally Invasive In-Utero Gastroschisis Repair.
- Best Poster award was given to researcher Andrew Lee from Anesthesiology for a poster on Use of the Baxter Faces (BARF) Scale to Measure the Severity of Nausea in Spanish Speaking Children.
Recipients of the 2017 Surgical Seed Grant Awards were announced as the grand finale of Texas Children’s Hospital Surgical Research Day. This grant program, funded by the Department of Surgery, allows surgery researchers to generate the preliminary data necessary for National Institutes of Health (NIH) grant applications and other extramural funding. Click here to find out who received a seed grant.
The Surgical Research Day Planning Committee included Dr. Jed Nuchtern (chair), Melinda Mathis (co-chair), Dr. Swathi Balaji, Shon Bower, Kathy Carberry, Dr. Jennifer Dietrich, Matthew Girotto, Laura Laux Higgins, Dr. Chester Koh, Dr. Lingkun Kong, Dr. Sandi Lam, Liz McCullum, Anissa Quiroz, Angie Rangel, Dr. Scott Rosenfeld, Stacy Staples and Veronica Victorian.