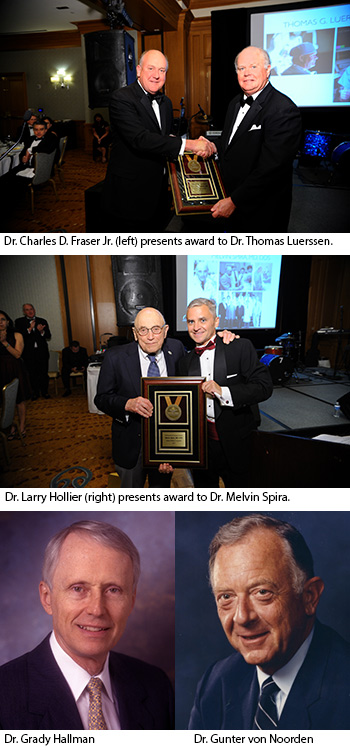
 The Texas Children’s Hospital Department of Surgery recently announced the recipients of the 2017 Distinguished Surgeon Award. The award is given to those who have forged a path of innovation in surgical excellence, research and education within the hospital’s Department of Surgery. Leaders in the department chose the recipients and announced this year’s winners on June 2 at the department’s annual dinner event. Two of the four award recipients were honored posthumously. All of the distinguished surgeons have significantly contributed to the legacy of the Texas Children’s Hospital Department of Surgery.
The Texas Children’s Hospital Department of Surgery recently announced the recipients of the 2017 Distinguished Surgeon Award. The award is given to those who have forged a path of innovation in surgical excellence, research and education within the hospital’s Department of Surgery. Leaders in the department chose the recipients and announced this year’s winners on June 2 at the department’s annual dinner event. Two of the four award recipients were honored posthumously. All of the distinguished surgeons have significantly contributed to the legacy of the Texas Children’s Hospital Department of Surgery.
This year’s Distinguished Surgeon Award winners are:
Dr. Grady L. Hallman (1930-2017)
In 1962, a young cardiovascular surgeon named Dr. Grady Hallman just out of cardiovascular surgical residency asked Dr. Denton A. Cooley, the founder of the newly established Texas Heart Institute, if he could join his practice and assist in his pioneering surgical work at Texas Children’s Hospital. Impressed with Hallman’s work, Cooley accepted him as his first associate at the Texas Heart Institute. Together, the surgeons collaborated for decades on innovative surgeries for children with congenital heart disease.
A native Texan born in Tyler, Hallman attended the University of Texas at Austin and graduated with honors. He went on to Baylor College of Medicine where he received a medical degree with honors in 1954, and was elected to the Alpha Omega Alpha Honor Medical Society. After serving his surgical residency in the Army Medical Corps, he returned to Baylor to complete his surgical training under Dr. Michael E. DeBakey. Hallman then joined Baylor’s Department of Surgery, when cardiovascular surgery was in its infancy. This is where he was introduced to Cooley.
The work between Cooley and Hallman led to many of the early advances in the field of congenital heart surgery and resulted in numerous publications, including the first comprehensive surgical textbook on the subject in 1966, Surgical Treatment of Congenital Heart Disease, and its revised editions published in 1975 and 1987. Hallman’s and Cooley’s other early contributions to the literature included journal articles on cardiovascular surgery in the first year of life; on congenital conditions such as coarctation of the aorta, tetralogy of Fallot, transposition of the great vessels, vascular rings, ventricular septal defects; and correcting congenital cardiovascular anomalies in adults. Throughout the course of his career Hallman authored 309 peer-reviewed papers.
Hallman was a member of many professional societies and gave generously of his time, serving as president of the Houston chapter of the American Heart Association, chairman of the membership committee of the Society for Thoracic Surgeons, and advisor to the State of Texas’ Crippled Children’s Services Program. He was the 1993-1994 Medical Honoree of the American Heart Association. Hallman was also honored as a Distinguished Alumnus of Baylor College of Medicine in 2003.
Dr. Thomas G. Luerssen
Dr. Thomas G. Luerssen is a neurosurgeon at Texas Children’s Hospital and professor of neurosurgery at Baylor College of Medicine. He was chief of Pediatric Neurosurgery at Texas Children’s from 2006 until 2016, and was Chief Quality Officer for Surgery from 2009 to 2017.
Luerssen attended Purdue University, graduating with a Bachelor of Science degree in 1973. He attended medical school at Indiana University, graduated in 1976, and completed his neurosurgery residency at Indiana University Medical Center. After residency, Luerssen entered private practice. His career in pediatric neurosurgery started in 1983 with fellowship training at the Children’s Hospital of Philadelphia under the direction of Dr. Luis Schut. After fellowship, Dr. Luerssen joined the faculty at the University of California San Diego. Working with Dr. Lawrence Marshall, he developed a clinical interest in pediatric neurotrauma which continued throughout his career. In 1988, he returned to Indiana University and spent 18 years as director of the pediatric neurosurgery service at the James Whitcomb Riley Hospital for Children.
In 2006, he was recruited as chief of Pediatric Neurosurgery at Texas Children’s to build upon the service started by Dr. William R. Cheek. Luerssen expanded the division by recruiting surgeons focused on subspecialties within pediatric neurosurgery. These subspecialties included: epilepsy, congenital abnormalities of the brain and spine, hydrocephalus, fetal conditions, neurotrauma and craniofacial abnormalities. He encouraged his faculty to apply innovative surgical techniques such as minimally invasive surgery and laser ablation that improved patient experience and surgical outcomes. He also saw the future of big data research and was an early proponent of value-based modeling.
At the time of his arrival, the hospital was completely revamping its Quality and Safety organizational structure. Luerssen was asked to undertake advanced training in quality improvement and patient safety. New positions of chief quality officers for medicine and surgery were created in 2009, and Luerssen was appointed chief quality officer for surgery.
In his quality position, Luerssen insistence on using data in an honest and transparent way to influence quality improvement laid the groundwork for many projects that are now considered standard operating procedure at Texas Children’s and the country. Among those are the pre-op time out, the use of surgical checklists, and the creation of the Surgical Quality Committee. He has also been a foundational participant in the hospital’s Daily Operational briefings version 1, 2 and now 3.0.
As one of the original partners on the Texas Children’s U.S. News & World Report project, Luerssen worked with the multidisciplinary teams to improve the quality of each service line as the ranking would follow the quality improvement. He has also been actively involved in the peer review process for surgeons on the Professional Practice Evaluation Committee at Texas Children’s.
He and his faculty at Texas Children’s and Indiana University have trained 18 fellows, most of whom remained in academic medicine. He has given more than 200 presentations at national forums and has published more than 200 articles or book chapters.
Dr. Melvin Spira
Dr. Melvin Spira served in the U.S. Navy during World War II where he completed his pre-dental studies. He graduated from Northwestern University Dental School with a dental degree in 1947. Soon after, he began practicing dentistry with his father in Chicago, IL. Called back to active duty in 1948, he served aboard the USS Philippine Sea and the USS Leyte where he had dental responsibilities for 700 Marines in the Mediterranean. After release to the reserves in 1950, he entered Northwestern University Graduate School intent on obtaining a master’s degree in oral surgery. However, he soon decided to focus on a career in plastic surgery. He spent three years in a general surgery residency at Duke University Medical Center and then completed his plastic surgery residency at Baylor College of Medicine in 1961, training at Jefferson Davis Hospital.
Spira joined the Plastic Surgery faculty at Baylor College of Medicine under Dr. S. Baron Hardy. When Hardy stepped down in 1976, Spira was appointed chief of Plastic Surgery by Dr. Michael E. DeBakey. Spira also served as chief of Plastic Surgery at Texas Children’s Hospital, Methodist Hospital, St. Luke’s Episcopal Hospital, the Veterans Affairs Medical Center in Houston and Ben Taub General Hospital. Spira retired as a full-time faculty member in 2003, moving to his home in Snowmass, Colo. He remained part of the Plastic Surgery faculty until his full retirement in 2012.
Beginning in the 1970s, Spira improved upon and developed microvascular surgery techniques used to reattach scalps, fingers, and eventually limbs. In addition, he did pioneering work with masseter-to-facial nerve transfers to reanimate facial muscles paralyzed by damaged facial nerves. The techniques he developed are still the standard used today. He also performed numerous surgeries to correct facial deformities, and improved on surgical techniques to correct clefts lips and palates, and associated nasal deformities. And he performed aesthetic cosmetic surgeries. In 1976, he was among the first physicians to call for Maxillofacial Surgery to be named as a distinct medical specialty.
During his career, Spira authored over 181 peer-reviewed articles published in many scientific journals, and authored 41 book chapters. For most of his professional career, and even after retirement, Spira volunteered with several organizations that sponsored surgical missions around the world. As an educator, Dr. Spira remained devoted to teaching the next generation of medical students and residents the important lessons he learned from his own professors and teachers.
Dr. Gunter K. von Noorden (1937-2017)
Dr. Gunter K. von Noorden was the first chief and founder of the Texas Children’s Hospital Department of Ophthalmology. He was known as one of the “fathers of pediatric ophthalmology” for his contributions to strabismus surgery and overall leadership in the field for more than 40 years.
Von Noorden committed his entire career to the study and treatment of strabismus and amblyopia. He was a pioneer researcher in the area of visual neurophysiology and transferred those new discoveries in strabismic and anisometropic amblyopia into improved clinical care. Through his relentless efforts and inspiration, ophthalmologists worldwide acquired new knowledge and understanding in pediatric ophthalmology and strabismus.
Born in Germany in 1928, Von Noorden’s family moved to Berlin in 1937. This had a profound impact on his life – exposing him to Adolf Hitler’s dictatorship and Nazi propaganda. Following his involvement in Battle of Berlin in 1945 and the end of WWII, Von Noorden was determined to dedicate his life to healing others, and he worked his way through medical school at the Johann-Wolfgang Goethe University.
Von Noorden began his medical career as a resident at the University of Iowa in 1957, which was followed by a fellowship at the University of Tuebingen Eye Clinic in Germany. He then returned to the University of Iowa, spending two years as an assistant professor of ophthalmology. In 1963, Von Noorden became a professor at the Wilmer Eye Institute at Johns Hopkins in Baltimore. In 1972, he moved to Houston to direct the Ocular Motility Service at Baylor College of Medicine.
Von Noorden was a professor of Ophthalmology and Pediatrics at Baylor, chief of the Ophthalmology Service at Texas Children’s Hospital, and adjunct professor of Neuroscience at the University of Texas at Houston from 1972 to 1995. Following an interval of retirement and appointment as professor emeritus, he rejoined Baylor as professor of Ophthalmology in July 2006 until October 2008. The Baylor Board of Trustees then appointed him Distinguished Emeritus Professor of Ophthalmology. Von Noorden passed away in Houston on February 18, 2017, at the age of 88.
In his lifetime, von Noorden published 310 scientific papers and authored 4 books, including Binocular Vision and Ocular Motility: Theory and Management of Strabismus. The book has been heralded as the “gold-standard text for ocular motility disorders.” He presented numerous lectures worldwide and received many honors.
In 2015, von Noorden was inducted in the American Society of Cataract and Refractive Surgery Hall of Fame as being “truly unique in his field and the ultimate triple threat: outstanding clinician, world-renowned teacher and author, and incredibly productive research scientist, highlighted by his path finding studies on the neuropathology of amblyopia.”
Drs. Hallman, Luerssen, Spira and von Noorden join the list of previous honorees, which includes: Dr. William Cheek, Dr. Denton Cooley, Dr. O.H. “Bud” Frazier, Dr. Ellen Friedman, Dr. Edmond Gonzales, Jr, Dr. Franklin Harberg, Dr. William Pokorny and Dr. David Wesson.














 Lynlee Boemer, a miracle baby who underwent fetal surgery performed at Texas Children’s Fetal Center to remove a large tumor (Sacrococcygeal Teratoma) growing from her spine, celebrated her first birthday on June 6.
Lynlee Boemer, a miracle baby who underwent fetal surgery performed at Texas Children’s Fetal Center to remove a large tumor (Sacrococcygeal Teratoma) growing from her spine, celebrated her first birthday on June 6.





 Seventeen-year-old Angelica Aulbaugh has been swimming since she was 4 years old. Her high level of training for a competitive team conditioned her to be tough, but nearly two years ago she noticed her left hand was swelling to an abnormal size.
Seventeen-year-old Angelica Aulbaugh has been swimming since she was 4 years old. Her high level of training for a competitive team conditioned her to be tough, but nearly two years ago she noticed her left hand was swelling to an abnormal size.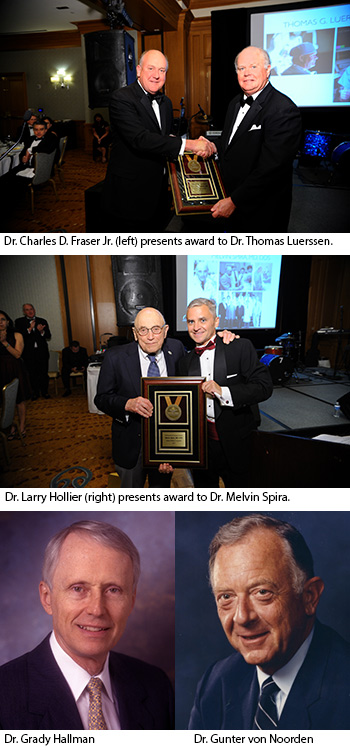 The Texas Children’s Hospital Department of Surgery recently announced the recipients of the 2017 Distinguished Surgeon Award. The award is given to those who have forged a path of innovation in surgical excellence, research and education within the hospital’s Department of Surgery. Leaders in the department chose the recipients and announced this year’s winners on June 2 at the department’s annual dinner event. Two of the four award recipients were honored posthumously. All of the distinguished surgeons have significantly contributed to the legacy of the Texas Children’s Hospital Department of Surgery.
The Texas Children’s Hospital Department of Surgery recently announced the recipients of the 2017 Distinguished Surgeon Award. The award is given to those who have forged a path of innovation in surgical excellence, research and education within the hospital’s Department of Surgery. Leaders in the department chose the recipients and announced this year’s winners on June 2 at the department’s annual dinner event. Two of the four award recipients were honored posthumously. All of the distinguished surgeons have significantly contributed to the legacy of the Texas Children’s Hospital Department of Surgery. An important milestone was recently reached at Texas Children’s Hospital that has one 17-year-old extremely grateful.
An important milestone was recently reached at Texas Children’s Hospital that has one 17-year-old extremely grateful.