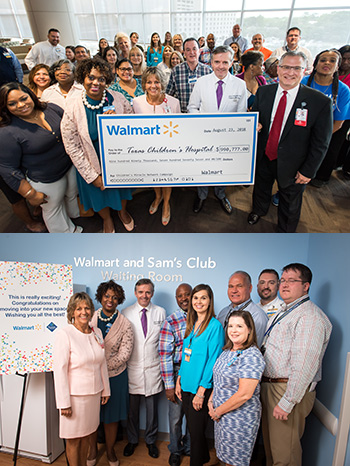
 On August 23, an excited group of Walmart and Sam’s Club employees visited Texas Children’s for a special presentation and ribbon cutting for the Walmart and Sam’s Club Waiting Room on the 20th floor of Legacy Tower and part of the new Texas Children’s Heart Center®. They were welcomed by Chief of Pediatric Cardiology Dr. Daniel Penny, Vice President Judy Swanson and Texas Children’s Executive Vice President Mark Mullarkey, who spoke about Texas Children’s special partnership with Walmart and Sam’s Club through the Children’s Miracle Network.
On August 23, an excited group of Walmart and Sam’s Club employees visited Texas Children’s for a special presentation and ribbon cutting for the Walmart and Sam’s Club Waiting Room on the 20th floor of Legacy Tower and part of the new Texas Children’s Heart Center®. They were welcomed by Chief of Pediatric Cardiology Dr. Daniel Penny, Vice President Judy Swanson and Texas Children’s Executive Vice President Mark Mullarkey, who spoke about Texas Children’s special partnership with Walmart and Sam’s Club through the Children’s Miracle Network.
“We couldn’t be more appreciative of the support we’ve had from Walmart and Sam’s Club over the years,” Mullarkey said. “Your generosity has made it possible for us to provide families with critically ill children the space they need to be together and to be comfortable.”
Even with a crowd of more than 30 attendees, there was plenty of room to move in the expansive new waiting area, which was specially designed as a haven for families with children who are dealing with some of the most complex medical issues – children like 11-year-old Jhett Skaggs, a Texas Children’s patient from Oklahoma, who with his dad, Brian, attended the event. Brian shared their story.
Jhett was born with cardiomyopathy, a rare heart disease. Doctors told Brian and his wife, Audra, that Jhett needed a life-saving heart transplant. They began researching options for treatment and decided Texas Children’s was the best choice. Experts from Texas Children’s flew to Oklahoma to transport Jhett to Houston, where he received a heart transplant at just 10 months old. For years, everything seemed to be okay, until at age 5 Jhett developed coronary artery disease. He would require another transplant. In 2012, Brian and Jhett moved to Houston to be closer to Texas Children’s. And though they had to wait nearly six years, Jhett finally received his second heart this past July.
“Everything worked out perfectly,” Skaggs said. “I wouldn’t change one single thing about our decision to come to Texas Children’s.”
After Brian’s moving story, Mullarkey turned the floor over to Trina Greer, Walmart Regional Vice President of Human Resources, who presented Texas Children’s with a check for nearly $1 million.
“It’s always my pleasure to watch our employees get excited about raising money for children who need our help,” Greer said. “I’m proud of the work we do and the funds we raise in the Greater Houston area to help Texas Children’s.”
Since 2005, Walmart and Sam’s Club have contributed more than $9.2 million. Last year, in addition to the funds raised in Houston area stores, the Walmart Foundation also gave Texas Children’s a gift of $500,000 for Hurricane Harvey Relief. In appreciation of this generosity, Texas Children’s leadership decided to dedicate the Heart Center’s new waiting area in honor of Walmart and Sam’s Club.
The new Heart Center – set to open on September 25 – will occupy eight floors and will feature four cardiac catheterization labs including integrated MRI scanner, four cardiovascular operating rooms, three cardiovascular ICU floors with 48 private rooms, two cardiac acute care floors with 42 private patient rooms, and a dedicated space for families.


















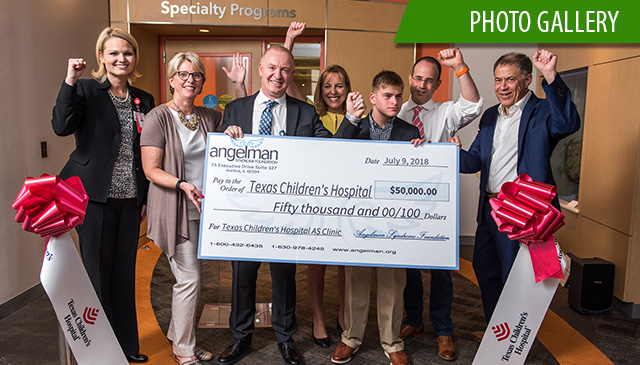 On July 9, Texas Children’s Hospital and the Angelman Syndrome Foundation celebrated the official opening of the Angelman Syndrome Clinic at Texas Children’s, one of only seven Angelman syndrome-specific clinics in the United States – and the first in Texas.
On July 9, Texas Children’s Hospital and the Angelman Syndrome Foundation celebrated the official opening of the Angelman Syndrome Clinic at Texas Children’s, one of only seven Angelman syndrome-specific clinics in the United States – and the first in Texas.















 When Kristine Hartin’s son was born almost a year ago, she was not prepared for the emergency cesarean section and almost four-week stay in the Neonatal Intensive Care Unit at Texas Children’s Hospital The Woodlands.
When Kristine Hartin’s son was born almost a year ago, she was not prepared for the emergency cesarean section and almost four-week stay in the Neonatal Intensive Care Unit at Texas Children’s Hospital The Woodlands.












