A little over a year ago, Larissa Fletcher took a huge leap of faith and walked into Texas Children’s Family Fertility Center to carry out the plan she and husband made years earlier on the darkest day of their lives.
On that dark day, Larissa and her late husband John Fletcher learned he had stage four esophageal cancer, and would, at best, live another year. Knowing they wanted to give their then 1-year-old daughter, Emma, a sibling, the couple decided to freeze John’s sperm and store it at the Fertility Center’s state-of-the-art in vitro fertilization (IVF) lab until Larissa was ready to try to have another child.
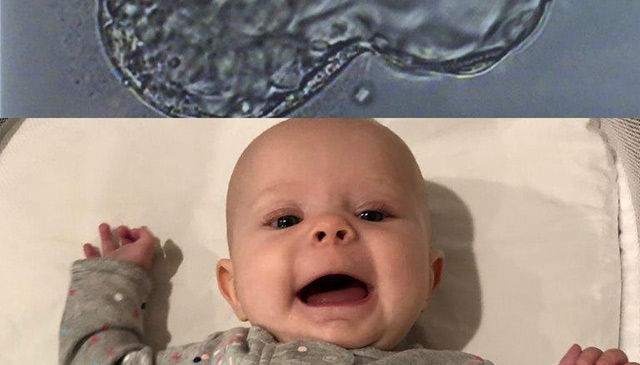
Shortly after that day came, Larissa watched her embryologist zoom her microscope in on what would become the now 4-month-old Elliana “Ellie” Joy Fletcher. Using a leading-edge embryo monitoring system called the EmbryoScope, Larissa also was able to watch a video of Ellie from when she was just a few cells all the way up to the time she was ready to be transferred into her mother’s belly to develop and grow for the next nine months.
“I was in awe of all of it,” Larissa said of the video. “In that moment, everything became very real for me.”
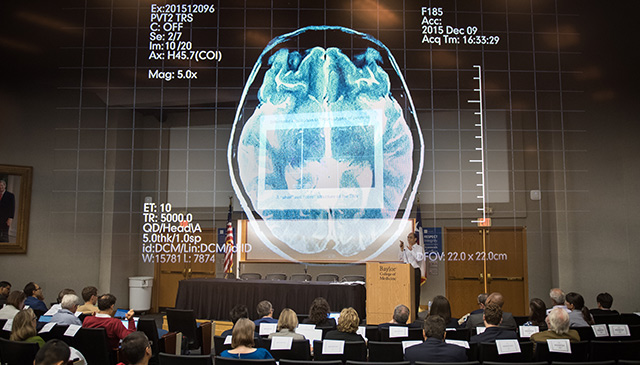
Texas Children’s Family Fertility Center’s three EmbryoScopes bring to life what reproductive endocrinology specialists see under a microscope and then describe to their patients. The technology, which provides continuous time-lapse imaging of embryos as they grow, also enables specialists to identify the healthiest embryo to transfer to the patient, for improved IVF success rates.
Dr. Richard Cochran, the Family Fertility Center’s Laboratory Director, said he and his colleagues in the lab are looking at whether the EmbryoScope can also help improve patient outcomes. The technology, he said, allows clinicians to see how an embryo divides, which in turn gives them the opportunity to see certain abnormalities.
“Sometimes embryos will divide, and then the cells will remerge, and then re-divide,” Cochran said. “That’s very abnormal, and that’s something we would not see in a traditional incubator setting.”
In such a setting, clinicians typically look at an embryo two days after fertilization is attempted, again a day or two later and so on. What happens in-between observations isn’t captured, and could be an important predictor of developmental abnormalities. For similar logistical reasons, the EmbryoScope already has proven to be helpful at enabling specialists to identify the healthiest embryo to transfer to a patient.
“In the vast majority of laboratories, embryos are put in traditional incubators where you have to take them out and expose them to room temperatures to see them,” said Texas Children’s Chief of Reproductive Medicine Dr. William Gibbons. “With the EmbryoScope, handling of the embryos is minimized and visibility is 24/7, enabling us to ensue embryos are growing and reach the appropriate stages at the appropriate times before transplantation.”
Texas Children’s Family Fertility Center is the only location in Texas other than Dallas that is using the EmbryoScope. The center has been using the technology since it opened in 2014 and currently has three. One of the scopes is dedicated to research while the other two are for clinical use.
Larissa, a former Fertility Center patient and a pediatrician with the Texas Children Newborn Center, said her experience at the center was extraordinary from beginning to beautiful end.
“When I was eight weeks pregnant and had to move my pregnancy care from the Family Fertility Center to a traditional OBGYN, it was bittersweet,” she said. “The people there were like my second family.”
To learn more about the EmbryoScope and how clinicians with the Texas Children’s Fertility Center uses the technology, click here.
Texas Children’s Family Fertility Center has earned national and international recognition for advancing the understanding and treatment of reproductive disorders. Our reproductive endocrinology specialists are proud of the impact we have made on the lives of our patients, women and families across the globe. To learn more about our Fertility Center, click here.