 Texas Children’s Transplant Services has hit another milestone – the completion of 200 lung transplants and 400 heart transplants, making the program one of the highest volume pediatric heart and lung transplant centers in the nation.
Texas Children’s Transplant Services has hit another milestone – the completion of 200 lung transplants and 400 heart transplants, making the program one of the highest volume pediatric heart and lung transplant centers in the nation.
The milestone continues to solidify Texas Children’s position as one of the most active pediatric transplant programs in the country, per the U.S. Department of Health & Human Services Organ Procurement and Transplantation Network.
“This type of volume has only been accomplished in a handful of pediatric programs across the United States,” Surgeon-in-Chief Dr. Larry Hollier said. “We are proud to add Texas Children’s Hospital to this distinguished list.”
Transplantation began at Texas Children’s in 1984 with a pediatric heart transplant. Since that time, liver, kidney and lung have been added and countless lives have been saved. Just last year, Texas Children’s Transplant teams performed 112 solid organ transplants, the most in the history of Texas Children’s Transplant Services.
“I’m proud to be working with a team so dedicated to providing the best possible outcomes for our patients,” said Dr. John Goss, medical director of Transplant Services. “This milestone demonstrates that Texas Children’s continues to earn its reputation as one of the best pediatric transplant programs in the country, and is a testament to the skill and commitment of our multidisciplinary team.”
Texas Children’s Transplant Services draws on numerous medical, surgical and support specialties, including transplant coordinators who play an essential role in connecting recipients with prospective donors, who ultimately made the transplant process possible.
“Without our donor families, our patients would not be given the gift that provides them a second chance at life,” said Dr. Jeff Heinle, surgical director of the Heart and Lung Transplant Program. “We can never forget to acknowledge the selfless decisions they make during the most difficult times of their lives.”
The recipients of Texas Children’s 200th lung transplant and 400th heart transplant are both doing well. Read more about their stories below as well as information about Texas Children’s Transplant Program and how to become an organ donor.
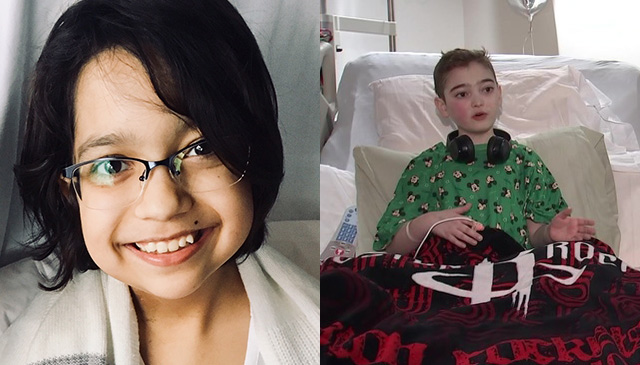
Brandon Cliff
Twelve-year-old Brandon Cliff has Cystic Fibrosis, a progressive genetic disease that causes lung infections, makes breathing difficult, and affects the pancreas, liver and other organs. The disease eventually leads to lung failure. Due to such complications, Brandon had been under consideration for a transplant for more than a year before receiving a double lung transplant on June 21. Performed by Dr. Iki Adachi, the transplant went well. Brandon was discharged from the hospital on July 3 and is ready to play with his brothers, cousins and friends as well as golf and basketball. Watch Fox 26’s news story about Brandon here.
Anacecilia Ortiz
Anacecilia Ortiz turned 14 at the beginning of July, just days after receiving her second heart transplant. The teenager got her first transplant at a children’s hospital in Colorado when she was 7 months old. Doctors there told her a transplant was necessary after finding a tumor inside her heart that was growing and could not be operated on. Over the years, Anacecilia’s body began to reject her new heart, causing it to develop scar tissue and not beat as hard as it should. A few serious dizzy spells earlier this year led Anacecilia’s physician in Brownsville to send her to Texas Children’s, where she was placed on the transplant list after trying medication. A month and a half later in mid-June, Anaceclila received her second heart transplant. Since then, she’s been doing extremely well and is currently recovering at her Pearland home.


 Texas Children’s Hospital was back on Capitol Hill in June in support of the Children’s Hospital Association Speak Now For Kids Family Advocacy Day, which brings patient families from around the United States to Washington, D.C. to share their experiences with lawmakers and staff, as well as to advocate for policies that will ensure the highest levels of medical care for children and their families.
Texas Children’s Hospital was back on Capitol Hill in June in support of the Children’s Hospital Association Speak Now For Kids Family Advocacy Day, which brings patient families from around the United States to Washington, D.C. to share their experiences with lawmakers and staff, as well as to advocate for policies that will ensure the highest levels of medical care for children and their families. “Thanks to online scheduling, it’s super easy to make appointments through MyChart now,” wrote a Texas Children’s family. “The past several times we’ve been here, we have been in and out in less than 45 minutes with the same level of quality and care. It seems like they heard our concerns loud and clear, and it shows that they care.”
“Thanks to online scheduling, it’s super easy to make appointments through MyChart now,” wrote a Texas Children’s family. “The past several times we’ve been here, we have been in and out in less than 45 minutes with the same level of quality and care. It seems like they heard our concerns loud and clear, and it shows that they care.” Scientists at Texas Children’s Hospital, Rice University and Baylor College of Medicine have won a prestigious National Institutes of Health grant to study the dynamic processes and cellular players linked to
Scientists at Texas Children’s Hospital, Rice University and Baylor College of Medicine have won a prestigious National Institutes of Health grant to study the dynamic processes and cellular players linked to 









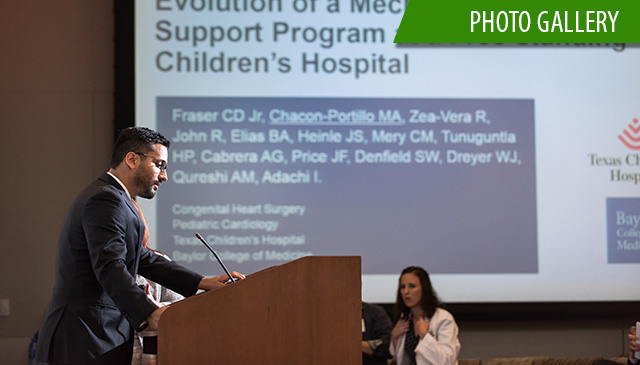 The Department of Surgery hosted the ninth annual Edmond T. Gonzales Jr. Surgical Research Day May 18 at Texas Children’s Pavilion for Women providing a forum for researchers across the department to showcase their work.
The Department of Surgery hosted the ninth annual Edmond T. Gonzales Jr. Surgical Research Day May 18 at Texas Children’s Pavilion for Women providing a forum for researchers across the department to showcase their work.















 The 2017 Texas Children’s Annual Report website highlighting last year’s growth and success with compelling stories, videos and graphics about our patients, staff, clinical programs and expanding facilities is here! This is the second time the Texas Children’s annual report has been released in a website format offering a dynamic representation of the breadth, depth and growth of our organization.
The 2017 Texas Children’s Annual Report website highlighting last year’s growth and success with compelling stories, videos and graphics about our patients, staff, clinical programs and expanding facilities is here! This is the second time the Texas Children’s annual report has been released in a website format offering a dynamic representation of the breadth, depth and growth of our organization.