
Last year, Texas Children’s Hospital The Woodlands celebrated its first year serving patients north of Houston and beyond, collecting praise from patients and families seeking expert care closer to home. Read more

Last year, Texas Children’s Hospital The Woodlands celebrated its first year serving patients north of Houston and beyond, collecting praise from patients and families seeking expert care closer to home. Read more

On April 26, superheroes of all sizes assembled on The Auxiliary Bridge to celebrate National Pediatric Transplant Week, observed each year during the last full week of National Donate Life Month in April.
The event, hosted by Texas Children’s Transplant Services, marked the end of a week that focuses on the powerful message of ending the pediatric transplant waiting list. There were plenty of fun activities for children, including karaoke, hula-hooping, coloring and crafts, a photo wall, and a visit from Elsa, one of Texas Children’s three therapy dogs. There were also educational materials available on organ donation and transplantation.
The event also honored real-life superheroes – the donor families whose children have saved and healed lives through organ, eye and tissue donation.
The gift of an organ transplant comes to one family as another family is enduring the most difficult time of their lives. The team in Transplant Services works hand in hand with Texas Children’s Spiritual Care Department during these times to provide donor families with compassionate support, to honor the choice to donate an organ, and to honor the legacy of the patient.
There are several ways we recognize the legacies of these children and their families, including:
In addition to these heartfelt moments of acknowledgement and remembrance, Texas Children’s Hospital has begun a new tradition to honor our donor families.
As the sun went down on April 22, Lester and Sue Smith Legacy Tower was illuminated in green and white. The tower was lit each evening for the rest of the week, both in commemoration of National Donate Life Month and Pediatric Transplant Week, and also as a tribute to our donor families. Going forward, the lighting of the tower will serve as yet another way Texas Children’s acknowledges them.
“Nothing we do would be possible without our donor families, and we wanted to find another way to honor them,” said Dr. John Goss, medical director of Transplant Services. “Now when people see Lester and Sue Smith Legacy Tower lit in green and white, they will know there’s a hero here at Texas Children’s who has just given the gift of life.”
Transplant Services at Texas Children’s was the nation’s largest pediatric transplant program in 2018, performing a remarkable 107 solid organ transplants including the highest volumes of pediatric liver, lung and kidney transplants.
Transplant Services provides a comprehensive, multidisciplinary approach to care through all aspects of the transplant process, from initial referral to hospitalization and outpatient management. Our team of experts includes physicians and surgical advanced practice providers, transplant coordinators, pediatric ventricular assist device coordinators, perfusionists, child life specialists, dieticians, social workers, financial counselors, pharmacists, inpatient and outpatient nursing and support staff, Perioperative Services, physical and occupational therapists, Radiology, Pathology, our LifeGift partners, and many others.
Our depth of skill and service enables us to offer world-class care for patients, from newborns to young adults, in need of heart, kidney, liver and lung transplants. That expertise has allowed us to successfully treat some cases that other national and international programs might consider untreatable.
Learn more about Transplant Services at Texas Children’s Hospital.
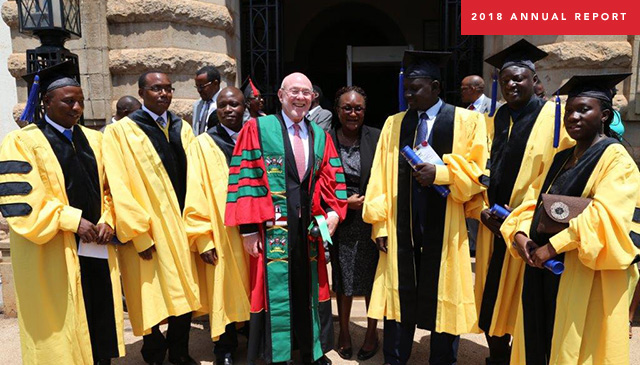
During its first year, the Global HOPE initiative made tremendous progress at creating an innovative pediatric hematology-oncology treatment network in sub-Saharan Africa. Learn more by visiting our 2018 virtual Annual Report.

On April 2, in celebration of World Autism Awareness Day, representatives from BBVA Compass Stadium, KultureCity and Texas Children’s Health Plan unveiled the Texas Children’s Health Plan Family Suite at a ribbon-cutting ceremony at the stadium.
Located in the northeast corner of the stadium outside of Section 220, the Texas Children’s Health Plan Family Suite includes a Sensory Room and a Mothers Room, making BBVA Compass Stadium the first sensory-inclusive facility in Major League Soccer. The Sensory Room was designed and installed in cooperation with KultureCity and Mothers Room at the BBVA Compass Stadium. KultureCity is the nation’s leading nonprofit dedicated to fight for inclusion and acceptance of all individuals, and advocates for those with sensory challenges such as autism and PTSD, just to name a few. It also provides training and equipment to public and private spaces in order to create an inclusive experience for everyone.
“KultureCity is truly honored to work with BBVA Compass Stadium and the Houston Dynamo to make them the first KultureCity Sensory-Inclusive MLS stadium. By recognizing this growing need and wanting to do something about it, they are truly putting their fans and guests first so that everyone regardless of their disabilities or sensory needs can be accepted and included,” said KultureCity co-founder Julian Maha, M.D. “This is a great day for the City of Houston and a great day for Major League Soccer in general. Thank you to the amazing team at the stadium and the entire Dynamo and Dash organization.”
The Mothers Room provides private space for mothers to nurse or pump while at the stadium and features seating for parent and child, as well as power outlets, a changing station and a television so mothers and children won’t miss a moment of game action.
In addition to the sensory room itself, the stadium will provide sensory bags created by KultureCity to guests who visit the space, and BBVA Compass Stadium and Houston Dynamo and Dash employees participated in sensory awareness training in order to understand how best to serve fans with unique needs and concerns.
“We take great pride in creating the most welcoming and inclusive atmosphere possible for all events at BBVA Compass Stadium, and we’re extremely excited about the addition of the Texas Children’s Health Plan Family Suite,” said Stadium Executive Vice President and General Manager Juan Rodriguez. “The Mothers Room will provide a private and comfortable space for women to care for their young children, and the Sensory Room affords fans with sensory needs the opportunity to step away if the sights and sounds inside the stadium become too much for them. We’re very grateful to the experts at KultureCity for their assistance in creating the space and training our staff.”
Since 2011, Texas Children’s Health Plan has been the official health insurance plan for Medicaid and the Children’s Health Insurance Program (CHIP) of the Houston Dynamo, Houston Dash and BBVA Compass Stadium. In addition to the new Texas Children’s Health Plan Family Suite, the health plan also sponsors the Texas Children’s Health Plan Family Section, located in Section 201 on the southwest corner of the stadium.
“We are proud to be a sponsor of the Houston Dynamo and are very excited to be part of the new Sensory Room and Mother’s Room at BBVA Compass Stadium,” Vice-President of Texas Children’s Health Plan Sherry Vetter said. “This innovative space is consistent with our mission to create a healthier future for children and women throughout our global community. The dedicated Mother’s Room gives nursing moms a private place to care for their infants while staying connected to the match and the Sensory Room provides a sensory-sensitive space for parents and children to enjoy and engage in matches on their terms.”

Dr. Richard Kellermayer, director of the Pediatric Inflammatory Bowel Disease program at Texas Children’s, has devoted much of his research to improving outcomes for children with chronic intestinal inflammation such as inflammatory bowel disease (Crohn’s disease and ulcerative colitis), as well as young patients who suffer from recurrent Clostridium difficile (C. diff) infections.
“C. diff is a bacterium that causes diarrhea and inflammation of the colon, which can be severe on occasions,” said Kellermayer, associate professor of Pediatrics at Baylor College of Medicine. “Some patients are susceptible to C. diff recurrences following repeated treatment with antibiotics. It can be increasingly challenging to successfully treat these patients with conventional methods.”
In a recently published paper in the Journal of Pediatric Gastroenterology and Nutrition, Kellermayer and his colleagues provide guidelines for the safe use of fecal microbiota transplantation to treat children with recurrent C. diff infections who are unresponsive to standard antibiotic treatments. This paper resulted from the collaborative efforts of leading experts in the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition (NASPHGAN) and the European Society for Pediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN).
Texas Children’s is among few hospitals across the nation exploring fecal microbiota transplantation (FMT), a nonconventional treatment that delivers stool from healthy donors into the colon of patients with C.diff in an attempt to restore a healthy, diverse bacterial population in the gut. C. diff infection is commonly associated with the microbial imbalance created in the gut due to frequent or prolonged use of antibiotics. This lack of microbial diversity allows the bacterium to grow excessively and produce toxins that cause diarrhea and other symptoms.
FMT has been used to manage recurrent C. diff infections in adult patients, with the cure rates approaching 90 percent. While it is not fully understood how FMT works, it is believed that the transfer of stool from a healthy donor helps repopulate the recipient’s gut with many kinds of beneficial bacteria, which discourages excessive growth of C. diff.
Kellermayer along with leading experts in the field noted in the paper that the incidence of C. diff infection among hospitalized, as well as healthy children in the community, has increased dramatically in the last decade. Pediatric patients can also have recurrent infections, similar to adults while being treated with C. diff directed antibiotics.
“Repeated and prolonged use of antibiotics in children may increase their risk of developing other gastrointestinal disorders later in life,” Kellermayer said. “So, better treatment options are urgently needed to treat children with recurrent C. diff infection, and FMT seems to provide a safe and effective treatment option for these patients at present. The collaboration between our IBD program and the Texas Children’s Microbiome Center, led by Drs. James Versalovic and Tor Savidge, provides an outstanding opportunity for us to advance FMT research. We are very grateful to our benefactors led by the Wagner and Klaasmeyer families, who support our research through the Gutsy Kids Fund.”
New study underway to analyze genetic implications of complicated pediatric Crohn’s disease
In a separate study funded by the Crohn’s and Colitis Foundation, Kellermayer and his research colleagues at Texas Children’s and Baylor College of Medicine will study the genetic background of complicated pediatric Crohn’s disease, a type of chronic, inflammatory bowel disease that can affect any part of the gastrointestinal tract.
“We will conduct high-throughput, genome wide genetic analysis on patients with Crohn’s disease to see if we can find any new genes that shed light on the most aggressive forms of the disorder and what makes certain people prone to developing it,” Kellermayer said. “If we know the genetic associations, we might find new means of prevention and treatment in the future.”
Almost seven years ago, surgeons with Texas Children’s Fetal Center performed their first in-utero neural tube defect repair surgery. Just a few months ago, some of those same surgeons reached a milestone when they completed their 100th neural tube defect repair.
Of the 100 total cases, more than half were performed fetoscopically, an experimental, minimally-invasive surgical approach pioneered at Texas Children’s in 2014 by Obstetrician and Gynecologist-in-Chief Dr. Michael Belfort and Pediatric Neurosurgeon Dr. William Whitehead.
Texas Children’s was the first center in the U.S. to correct neural tube defects, also known as spina bifida defects, fetoscopically and is among just a few centers in the country that offers fetoscopic repair of spina bifida. Texas Children’s continues to offer open fetal surgery for spina bifida, the standard of care since 2012, for patients who do not qualify for or opt not to undergo a fetoscopic repair.
“This milestone shows that we are a mature program, that we have done a lot of these cases, and that our results are equivalent if not better, than anybody else out there doing this,” Belfort said. “We have a level of experience now whereby we can assure patients and families that what we offer is the best in terms of quality and safety.”
Neural tube defect repair surgeries are performed on babies with Myelomeningocele, a developmental defect in which the spine is improperly formed and the spinal cord is open to and fused with the skin. The condition, also known as spina bifida or an open neural tube defect (NTD), occurs in 3.4 out of every 10,000 live births in the U.S. and is the most common permanently disabling birth defect for which there is no known cure.
NTDs are usually associated with motor impairment and hydrocephalus, or the buildup of cerebrospinal fluid in the brain, which requires surgical treatment to drain the fluid via an implanted device called a shunt. It’s common for children with spina bifida to have abnormal function of their bladder, bowels and legs. The goal of fetal surgical repair of spina bifida is to preserve leg function and reduce the need for a postnatal shunt.
The standard of care for spina bifida is neurosurgical closure of the defect in the first days of life, however, advances in fetal surgery and the landmark clinical trial, known as the Management of Myelomeningocele Study (MOMS Trial), proved that a fetal surgical repair leads to decreased rates of hydrocephalus and improved leg function compared to a postnatal repair.
Through their research and outcomes data, Belfort and his team have shown that performing the surgery fetoscopically yields the same outcome for the baby as the open repair, while being significantly less invasive for the mother.
“We are thrilled to offer this innovative and minimally-invasive surgical approach to our patients and their babies,” Belfort said. “We thank the mothers and families who put their trust in our team and have the courage to undergo an experimental procedure.”
The first mother to undergo fetoscopic neural tube repair at Texas Children’s Fetal Center was Althea Canezaro. At 23 weeks pregnant, Althea learned during a routine ultrasound that her son, Grayson, had spina bifida. The Louisiana resident came to Texas Children’s shortly thereafter and met with Belfort and his team.
“After talking with them, it was like, OK, there’s something they can do for us, and if it didn’t work out everyone would be safe,” Althea recalled. “We knew that this was an opportunity to give him the best life that he could have. So, going forward, it was kind of like the ball was in their park. The weight was taken off our shoulders.”
A little more than four years later, Althea and Grayson are thriving. The blonde haired, blue-eyed boy never developed hydrocephalus and was born with full movement of his legs. He is hitting all of his developmental milestones and walks with and without the assistance of crutches.
“He’s a fighter,” Althea said. “You can’t tell him he can’t do anything. He has more determination than you ever want to believe.”
Belfort and his team performed the 100th neural tube defect repair late last year and delivered the healthy little girl, Parker Kate, on March 5. Taylor Avera, the newborn’s mother, said when she and her husband found out their child had spina bifida they were scared to death, but that what they learned at Texas Children’s put them at ease.
“Neither one of us questioned that this was what we needed to do,” Taylor said. “We were excited that we were candidates for the surgery and that we were going to be able to give our baby the best outcome she could have.”
The experimental surgery Althea and Taylor underwent continues to be subject to rigorous oversight by the U.S. Food and Drug Administration, was developed by Texas Children’s Fetal Center in partnership with Texas Children’s division of neurosurgery. The teams practiced on a child’s kickball that replicated the mother’s uterus. Inside the kickball, a doll acted as the fetus. By hoisting the ball into the air hung by various levers and pulleys, the team simulated the movement in the womb and practiced closing the spinal cord.
“The multidisciplinary collaboration with the Fetal Center on this surgical effort is an extraordinary example of the innovative spirit at Texas Children’s Hospital,” Whitehead said. “From a medical standpoint, we believe by closing the defect both in-utero and fetoscopically, is a less invasive procedure for the mother, reduces her risk of preterm delivery and reduces the need for shunts.”
View photos of both Grayson and Parker Kate below.
Texas Children’s Fetal Center is among the nation’s leaders in providing high-risk maternal care and the diagnosis and treatment of abnormalities in unborn and newborn infants. For more information, visit women.texaschildrens.org/fetal.

Just months after successfully expanding our spine surgery program outside the medical center, the Department of Surgery and Texas Children’s Hospital The Woodlands are celebrating another important milestone – the expansion of our bariatric surgery services.
“We are very pleased about the collaboration between all services in opening up the bariatric surgery program at our campus in The Woodlands,” said Surgeon-in-Chief Dr. Larry Hollier. “The Department of Surgery is committed to bringing the surgical services that families need closer to their homes.”
Previously, access to bariatric surgery was relegated to our Texas Medical Center campus. However, a review of comparative patient data and geographic analysis revealed that a large number of patients coming to Texas Children’s for bariatric surgery were coming from The Woodlands and other communities outside Houston. With support from Texas Children’s executive leadership and Department of Surgery leadership, a multidisciplinary team in The Woodlands began laying the groundwork to expand the program.
“Successfully setting up bariatric surgery in The Woodlands required extensive planning and coordination on many fronts,” said Ketrese White, assistant vice president at Texas Children’s Hospital The Woodlands. “In addition to putting necessary infrastructure in place – such as personnel, equipment and surgical space – and running simulations, this amazing team spent months mapping out optimum workflow processes, including solidifying how we identify patients and establishing a rigorous assessment plan.”
The pre-surgery assessment period for bariatric surgery is lengthy – usually six to eight months. In addition to meeting physical criteria, candidates must also undergo diagnostic testing, attend regular clinic visits, and receive lifestyle and diet education.
“We’ve been very thoughtful in developing our assessment criteria,” White said. “The team performed due diligence, reviewing best practices and consulting experts both inside and outside the Texas Children’s system, which has also helped us build relationships in the community.”
The hard work paid off. Last month, pediatric surgeon Dr. Shawn Stafford performed the first bariatric surgeries at Texas Children’s Hospital The Woodlands, the culmination of months of collaboration and preparation.
The expansion of our bariatric surgery services in The Woodlands helps us meet a major need in the community. Obesity-related health problems doctors once saw only in middle-aged people are now being seen in teenagers. These conditions include high blood pressure, type 2 diabetes, polycystic ovarian syndrome, obstructive sleep apnea, severe bone and joint issues, and hepatosteatosis (fatty liver), not to mention increased risk of heart attack and cancer.
“We have a unique opportunity to intervene and head off potentially debilitating, or even fatal chronic medical conditions, and ultimately to help make a lasting difference in these kids’ lives,” Stafford said.
Because each of these cases is so different, Texas Children’s experts put special emphasis on building a program of care around each unique patients’ needs, even helping tailor an exercise regimen based on their lifestyle and interests.
“Our goal is to communicate with each patient and find things they enjoy doing so that the changes they’re making to their lifestyle will be durable,” Stafford said.
While bariatric surgery isn’t a cure for obesity, Stafford says it is a valuable tool that makes victory against obesity a possibility. But changing a lifestyle still requires effort.
“I like to describe it as if they are trying to get over a wall: I can’t make them go over, but I can give them a boost so that, if they choose, they can pull themselves over.”
Learn more about bariatric surgery at Texas Children’s.