Just before Father’s Day, 14-year-old Gage Lipscomb received a gift from his father like no other – a kidney.
Just before Father’s Day, 14-year-old Gage Lipscomb received a gift from his father like no other – a kidney.
On June 14, Dr. Richard Link, medical director of living donor kidney transplant at Baylor St. Luke’s Medical Center, removed David Lipscomb’s left kidney and released it to the transplant team at Texas Children’s Hospital.
During a six-hour procedure, Dr. Christine O’Mahony, surgical director of kidney transplantation at Texas Children’s Hospital, transplanted Lipscomb’s kidney into Gage, the youngest boy of 10 siblings.
Gage was diagnosed with solitary kidney as a baby and was placed on medication following the removal of his right kidney at a young age. For many years, Gage experienced a seemingly typical childhood, excelling in academics and devoting his free time to playing soccer, baseball and basketball. But recently, his health started to decline.
“He was not yet on dialysis, but if he didn’t get a kidney transplant soon, he would have had to have gone on dialysis,” O’Mahony said.
So Gage’s dad stepped up and became his donor.
Early Wednesday morning while the teen was being prepped for surgery at Texas Children’s, his dad was in a nearby operating room at St. Luke’s having laparoscopic surgery – a minimally invasive operation – to remove his kidney.
“The two hospitals are attached,” said O’Mahony. “Dr. Link, the urologist who took out the kidney in David, started around 8 a.m. in the morning.”
The timing of the two events is important.
“We want to minimize the time between the kidney coming out of the donor and implanting it into the patient. I walked over to St. Luke’s to help take out David’s kidney with Dr. Link. The kidney still had blood in it so we had to flush the blood out,” O’Mahony said.
Then, she said, “We literally packed it up in a cooler so it stays cold and walked back to Texas Children’s and unpacked it” and “sewed” David’s kidney inside of Gage.
The father and son are doing well and spent a very special Father’s Day recovering and giving thanks for the opportunity to undergo this life-altering operation.
“I’m glad you are my dad,” Gage told his father during one of their hospital room visits. “Thanks.”
David said giving Gage his kidney was the least he could do and that knowing his son is going to be OK is the best Father’s Day gift he could ever have.
To read and watch news coverage of the living donor transplant, click any of the links below. For more information on Texas Children’s Transplant Services click here.
Just before Father’s Day, dad donates kidney to 1 of 10 children (CBSNews.com)
ABC World News Tonight Facebook post
Dad’s priceless gift to son (Houston Chronicle)
Father donates kidney, saves 14-year-old son’s life (CBS 11 KHOU)
Father donates kidney to 14-year-old son who had kidney removed (ABC 13 KTRK)


 Lynlee Boemer, a miracle baby who underwent fetal surgery performed at Texas Children’s Fetal Center to remove a large tumor (Sacrococcygeal Teratoma) growing from her spine, celebrated her first birthday on June 6.
Lynlee Boemer, a miracle baby who underwent fetal surgery performed at Texas Children’s Fetal Center to remove a large tumor (Sacrococcygeal Teratoma) growing from her spine, celebrated her first birthday on June 6.





 Seventeen-year-old Angelica Aulbaugh has been swimming since she was 4 years old. Her high level of training for a competitive team conditioned her to be tough, but nearly two years ago she noticed her left hand was swelling to an abnormal size.
Seventeen-year-old Angelica Aulbaugh has been swimming since she was 4 years old. Her high level of training for a competitive team conditioned her to be tough, but nearly two years ago she noticed her left hand was swelling to an abnormal size.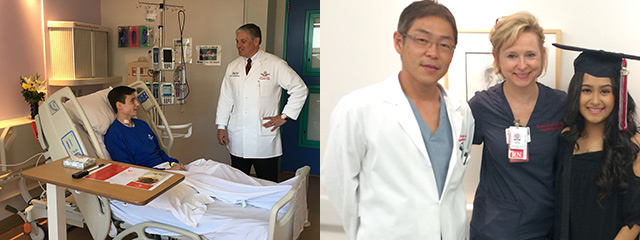 An important milestone was recently reached at Texas Children’s Hospital that has one 17-year-old extremely grateful.
An important milestone was recently reached at Texas Children’s Hospital that has one 17-year-old extremely grateful.