February 27, 2022

Sunday, February 27, 2022: 8:16 a.m.
Timekeeping Adjustment Forms due by 10 a.m. Monday, Feb. 28
Texas Children’s Team Members,
Monday, Feb. 28 at 10 a.m. is the deadline to submit and leaders to approve Timekeeping Adjustment Forms for all previous pay periods during the Kronos outage. After that time, any adjustments to previous pay periods during the Kronos outage will require SVP approval.
While we have strived to reduce timekeeping errors following the Kronos outage, we do commit to capturing and compensating for adjustments as quickly as possible.
- Do not submit an adjustment without first reviewing your paycheck in MOLI. Paychecks for the pay period ending Feb. 19 are now available in MOLI.
- You can now view your previously processed Timekeeping Adjustment Forms by clicking the View My Adjustments button in Connect Clock. This information is updated weekly. Review these, as well as your previous paychecks in MOLI, before submitting an adjustment. If you have already submitted an adjustment request please do not resubmit.
- In Connect Clock, employees can now view their accrual calculations for PTO, EIB and My Day for each pay period (through Feb. 19) during the outage by clicking the Outage Accrual Calculations button. All employees have this functionality and leaders are able to view their employees’ calculations as well. Please review this data carefully before submitting Timekeeping Adjustment Forms.
- When submitting the form, focus only on incremental (additional) amounts of hours to be paid for and not the total number of hours worked.
- If an employee is unable to submit an adjustment form, their leader can submit on their behalf.
If you have questions after reviewing your data and updated balance in Kronos (available tomorrow), and believe your accrual balance is incorrect, please send an email to payroll@texaschildrens.org.
Thank you for continued patience during the Kronos outage. For more information, visit our Connect Resources site.
Lovie Ross
Director, Financial Disbursements, Finance
Arlene Hillegeist
Director, Compensation, Human Resources
Monday, February 21, 2022: 9:47 a.m.
Timekeeping Adjustment Forms due by 10 a.m. Monday, Feb. 28
Texas Children’s Team Members,
Monday, Feb. 28 at 10 a.m. is the deadline to submit and leaders to approve Timekeeping Adjustment Forms for all previous pay periods during the Kronos outage. After that time, any adjustments to previous pay periods during the Kronos outage will require SVP approval.
While we have strived to reduce timekeeping errors following the Kronos outage, we do commit to capturing and compensating for adjustments as quickly as possible.
- Do not submit an adjustment without first reviewing your paycheck in MOLI.
- You can now view your previously processed Timekeeping Adjustment Forms by clicking the View My Adjustments button in Connect Clock. This information is updated weekly. Review these, as well as your previous paychecks in MOLI, before submitting an adjustment. If you have already submitted an adjustment request please do not resubmit.
- When submitting the form, focus only on incremental (additional) amounts of hours to be paid for and not the total number of hours worked.
- If an employee is unable to submit an adjustment form, their leader can submit on their behalf.
Thank you for continued patience during the Kronos outage. For more information, visit our Connect Resources site.
Lovie Ross
Director, Financial Disbursements, Finance
Arlene Hillegeist
Director, Compensation, Human Resources
Monday, February 21, 2022: 6:01 a.m.
KRONOS IS LIVE!
Texas Children’s Team Members,
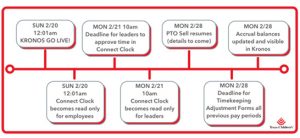
We are happy to announce, Kronos is live. Please use Kronos to clock in/out and request time off. Below are two key reminders as we transition from Connect Clock.
- TIME OFF. We are in the process of updating your PTO and EIB balances to reflect the use and accrual of these banks during the Kronos outage, and they will be available in Kronos on Feb. 28. Until that time, please refer to your most recent accrual balance in Connect Clock before submitting time off requests. If your leader approves your request and you do not have the hours available, you will not be paid for that time off, so please pay close attention to your available balances. If you requested time off for after Feb. 20, you will need to resubmit those requests in Kronos.
- TIMEKEEPING. Please ensure your time is accurate in Connect Clock as leaders will need to review and approve your time by 10 a.m. Feb. 21 for the pay period ending Feb. 19. The deadline to submit and your leader to approve Timekeeping Adjustment Forms for all previous pay periods during the Kronos outage is Monday, Feb. 28. After that time, any adjustments to previous pay periods during the Kronos outage will require SVP approval.
To access a detailed FAQ document regarding the transition, please click here. For additional support, please contact your leader.
If you have any issues logging in to Kronos on computers, please contact the IS Helpdesk. If your Kronos clock does not work, please contact Payroll.
Thank you for your patience and partnership throughout the Kronos outage.
Josh Ashlock
Administrator on Call
Michelle Riley-Brown
EVP on Call
Sunday, February 20, 2022: 8:46 a.m.
KRONOS IS LIVE!
Texas Children’s Team Members,
We are happy to announce as of 12:01 a.m. today, Kronos is live. Please use Kronos to clock in/out and request time off. Below are two key reminders as we transition from Connect Clock.
- TIME OFF. We are in the process of updating your PTO and EIB balances to reflect the use and accrual of these banks during the Kronos outage, and they will be available in Kronos on Feb. 28. Until that time, please refer to your most recent accrual balance in Connect Clock before submitting time off requests. If your leader approves your request and you do not have the hours available, you will not be paid for that time off, so please pay close attention to your available balances. If you requested time off for after Feb. 20, you will need to resubmit those requests in Kronos.
- TIMEKEEPING. Please ensure your time is accurate in Connect Clock as leaders will need to review and approve your time by 10 a.m. Feb. 21 for the pay period ending Feb. 19. The deadline to submit and your leader to approve Timekeeping Adjustment Forms for all previous pay periods during the Kronos outage is Monday, Feb. 28. After that time, any adjustments to previous pay periods during the Kronos outage will require SVP approval.
To access a detailed FAQ document regarding the transition, please click here. For additional support, please contact your leader.
If you have any issues logging in to Kronos on computers, please contact the IS Helpdesk. If your Kronos clock does not work, please contact Payroll.
Thank you for your patience and partnership throughout the Kronos outage.
Mike Brown
Administrator on Call
Weldon Gage
EVP on Call
Friday, February 18, 2022: 9:21 a.m.
Kronos Go Live scheduled for Feb. 20
Texas Children’s Team Members,
We are going back in time! Mark your calendars, as Kronos and our regular timekeeping practices will begin at 12:01 a.m. Sunday, Feb. 20.
To make this process as smooth as possible, we want to provide three key things you need to know as we prepare for the transition.
- TIMELINE. Please continue to use Connect Clock to clock in/out through Saturday, Feb. 19. For any shifts beginning after 12:01 a.m. Feb. 20, use Kronos to clock in/out and request time off as you had before. Access to Kronos will be available on clocks, computers and the mobile app.
For employees working a shift that begins Feb. 19 and ends Feb. 20, please clock in using Connect Clock, but do not clock out using either system. Instead, inform your leader so they can add your clock out time in Connect Clock for the pay period ending Feb. 19 when they do their final review and approval. If you take a break after 12:01 a.m., you also should not clock in and out for that meal break in Kronos. Please inform your leader of your clock out/in times and they will enter the time in Connect Clock.
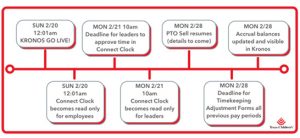
- TIME OFF. When Kronos goes live, we will need some time to update your PTO and EIB balances to reflect the use and accrual of these banks during the Kronos outage. The updated balances will not be available and shown in Kronos until Feb. 28. Until that time, as no accrual balances will appear in Kronos, please refer to your most recent accrual balance in Connect Clock before submitting time off requests. If your leader approves your request and you do not have the hours available, you will not be paid for that time off, so please pay close attention to your available balances. If you requested time off for after Feb. 20, you will need to resubmit those requests in Kronos at go live.
- TIMEKEEPING. Please ensure your time is accurate in Connect Clock as leaders will need to review and approve your time by 10 a.m. Feb. 21 for the pay period ending Feb. 19. The deadline to submit and your leader to approve Timekeeping Adjustment Forms for all previous pay periods during the Kronos outage is Monday, Feb. 28. After that time, any adjustments to previous pay periods during the Kronos outage will require SVP approval. Later today, you can access your list of paid off-cycle adjustments by clicking the View My Adjustments button in Connect Clock. Please see FAQ for more information.
To access a detailed FAQ document regarding the transition, please click here. For additional support, please contact your leader.
At go live, if you have any issues logging in to Kronos on computers, please contact the IS Helpdesk. If your Kronos clock does not work, please contact Payroll.
Thank you for your patience and partnership as we navigated timekeeping and payroll processes during the Kronos outage and as we transition back to our routine timekeeping practices.
Mike Brown
Administrator on Call
Weldon Gage
EVP on Call
Tuesday, February 15, 2022: 6:45 p.m.
Kronos Restoration Scheduled for Feb. 20
Texas Children’s Team Members,
Today, we are pleased to announce we are going back in time! Mark your calendars, as our transition back to Kronos and our regular timekeeping practices will begin at 12:01 a.m. Sunday, Feb. 20. Although we have thoroughly tested the system, this date is still subject to change. If this occurs, we will update you in a subsequent global communication.
To make this process as smooth as possible, we want to provide three key things you need to know as we prepare for the transition.
- TIMELINE. Please continue to use Connect Clock to clock in/out through Saturday, Feb. 19. For any shifts beginning after 12:01 a.m. Feb. 20, use Kronos to clock in/out and request time off as you had before. Both the Kronos clocks and Kronos on computers will be available for full use.
For employees working a shift that begins Feb. 19 and ends Feb. 20, please clock in using Connect Clock, but do not clock out using either system. Instead, inform your leader so they can add your clock out time in Connect Clock for the pay period ending Feb. 19 when they do their final review and approval.
- TIME OFF. When Kronos goes live, we will need some time to update your PTO and EIB balances to reflect the use and accrual of these banks during the Kronos outage. The updated balances will not be available and shown in Kronos until Feb. 28. Until that time, please refer to your most recent accrual balance in Connect Clock before submitting time off requests. If your leader approves your request and you do not have the hours available, you will not be paid for that time off, so please pay close attention to your available balances. If you requested time off for after Feb. 20, you will need to resubmit those requests in Kronos at go live.
- TIMEKEEPING. Please ensure your time is accurate in Connect Clock as leaders will need to review and approve your time by 10 a.m. Feb. 21 for the pay period ending Feb. 19. The deadline to submit and your leader to approve Timekeeping Adjustment Forms for all previous pay periods during the Kronos outage is Monday, Feb. 28. After that time, any adjustments to previous pay periods during the Kronos outage will require SVP approval.
To access a detailed FAQ document regarding the transition, please click here. For additional support, please contact your leader.
Thank you for your patience and partnership as we navigated timekeeping and payroll processes during the Kronos outage and as we transition back to our routine timekeeping practices.
Mike Brown
Administrator on Call
Weldon Gage
EVP on Call
Thursday, January 20, 2022: 8:30 a.m.
Accrual balances now available in Connect Clock
Texas Children’s Team Members,
Starting today, employees can now view their accrual balances in Connect Clock. These balances reflect accruals earned in accordance with the organization’s time off policy less any time off taken during the Kronos outage. Please review these balances carefully before submitting any time off requests to ensure you have enough hours available to take. If you request time off and do not have a sufficient balance, your leader will need to enter time as ANP (absent not paid).
Please review the details below.
- Not updated in real time. The accruals do not represent real-time data and will only be updated after each pay period. The current data reflects accruals as of the previous pay period ending Jan. 8. Any time off approved since then will not be reflected until the beginning of the next pay period starting Jan. 23.
- PTO sells. Since we are unable to process PTO sells at this time, employees are allowed to accrue over the maximum limits. This practice will be discontinued after Kronos is restored, following an opportunity to sell PTO.
- Per diem and part-time employees. If you are in this group of employees, the banks may not be accurate as the resources are unavailable to confirm status or effective date. Please double check your manual sheets to ensure you’re following an accurate balance.
- Balance inquiries. If you have any questions on your accrual balances, please contact timekeeping@texaschildrens.org.
Thank you for your patience and partnership during this Kronos outage.
Eric Allum
Administrator on Call
Dan DiPrisco
EVP on Call
Friday, January 14, 2022: 3:20 p.m.
Kronos Outage Update: Connect Clock Accessibility
Texas Children’s Team Members –
Earlier today, some of our Texas Children’s employees encountered issues with being able to access Connect Clock to perform their required timekeeping functions. At this time, Connect Clock is performing as usual; however, our IS team is still working to identify the root cause of the temporary outage.
In the meantime, if you were impacted by this issue, please support by taking the following actions:
- Continue to use Connect Clock to complete all required timekeeping for today. Follow the sequence of clocking in and out for your shift and meal break.
- Notify your leader of any incorrect punch times. To make this easy, employees can view their punch times in Connect Clock. To message your leader about a correction, please click the Envelope under “Get Help” next to the date with the error and detail the correct times in the email template that opens.
- For Leaders, please correct any timekeeping errors as soon as possible to ensure hours are inputted correctly. Any day with missed punches or punch errors will be shown in red in Connect Clock.
In the event the issue returns, employees may also utilize our Manual Tracking Sheet to help with recording time. For other information about the Kronos outage, visit our Connect site.
Thank you for your patience in this matter. We will communicate updates as more information becomes available.
Jackie Ward
Administrator on Call
Mark Mullarkey
EVP on Call
Sunday, January 9, 2022: 8 a.m.
Kronos Outage Update: Approval deadline tomorrow at 10 a.m.
Texas Children’s Team Members,
With the close of our latest pay period over the weekend, leaders now have until 10 a.m. tomorrow to approve their employees’ time in Connect Clock. This includes clock in/out times, time off and any applicable pay programs. After this deadline, there will be no more opportunities to make changes prior to the issuance of this week’s paycheck, which will be taking place on our normal schedule.
For more information on this process, please see below.
- Check your hours before the deadline. Using the View My Times feature within Connect Clock, review your punches for the current pay period. Please look over your times according to your manual tracking sheet, and if you identify an error, please work with your leader prior to the 10 a.m. Monday deadline to correct any discrepancies.
- Adjustments due for previous pay periods. To ensure everyone is focused on reviewing and approving time for the current pay period, please submit any Timekeeping Adjustment Forms for the pay periods ending Dec. 11 and 25. If you are awaiting an adjustment to be processed, please do not resubmit another form.
Thank you for your flexibility and patience as we continue to work through solutions together.
Shannon Zerber
Administrator on Call
Weldon Gage
EVP on Call
Thursday, January 6, 2022: 4:05 p.m.
Kronos Outage Update: Connect Clock Enhancements and Reminders
Texas Children’s Team Members,
As we continue to navigate the Kronos outage, our priority remains compensating our employees on time and correcting any discrepancies as quickly as possible. To help achieve this goal, we have added functionality into Connect Clock to make it easier for you to track time, request time off and fix any errors.
- View My Times screen. When you select View My Times, you will see a list of each day’s punches or single events (i.e., PTO). The list is color coded: green is approved, white is action needed and red indicates there is an issue (i.e., missed punch). Your leader will also have a similar view. Please click here for a screen shot.
- Request time off. Both exempt and non-exempt employees now have the ability to request time off in Connect Clock and leaders can approve it. Please do not resubmit previously submitted time off to avoid duplicate entries in Connect Clock. Please click here for instructions.
Please note: If you currently enter time off in Clairvia, you will need to request time off in both Clairvia and Connect Clock until further notice.
- Message your leader. To help reduce timekeeping errors, there is a new optional feature allowing you to send an email notification to your leader for a particular time entry. In the View My Times new screen, there is an envelope icon at the end of each line. If you click this button, it will send an email to your leader. Please add in specific detail on your email request, so they can better assist you.
- Overpayments. Although Texas Children’s will not recoup overpayments for the pay period ending Dec. 11, as we now have the ability to track time through Connect Clock, we will work to recoup overpayments starting with the pay period ending Dec. 25. If you notice an overpayment in your paycheck, please submit a Timekeeping Adjustment Form. If the overpayment is due to inputting an incorrect pay code, please include a negative amount for the incorrect pay code and add the new pay code using a positive amount. If there was another cause for the overpayment, please indicate the overpayment amount as a negative number.
- Adjustment deadline for previous pay periods. To ensure everyone is focused on reviewing and approving time in the current pay period, please submit any Timekeeping Adjustment Forms for the pay periods ending Dec. 11 and 25 by 10 a.m. Monday, Jan. 10. If you are awaiting an adjustment to be processed, please do not resubmit another form.
- PTO Sells. Due to the Kronos outage, we are currently unable to process PTO sells at this time. We will continue to review options and communicate once we have more information.
- Need Help? For support during this event please call the Employee Support Center at 832-826-4700. The line will be open Monday through Friday from 7 a.m. to Noon. You may also email any time at hremployeesupportcenter@texaschildrens.org.
Thank you for your partnership and patience as we continue to navigate the Kronos outage. We will continue to update you on any future enhancements to make this process more efficient and accurate.
Shannon Zerber
Administrator on Call
Weldon Gage
EVP on Call
Sunday, January 2, 2022: 2:10 p.m.
Kronos Outage Update: Timekeeping Adjustment forms due by tomorrow at 10 a.m.
Texas Children’s Team Members,
Tomorrow by 10 a.m. is the deadline to have any Timekeeping Adjustment Forms approved by your leader to be processed in time for our next off-cycle payroll distribution, taking place Jan 6 (when it appears in an account will be dependent on the employee’s bank). Please ensure you submit adjustments as soon as possible to give your leader time to review and approve.
While we have strived to reduce timekeeping errors following the loss of Kronos, we do commit to capturing and compensating for adjustments as quickly as possible.
- Do not submit an adjustment without first reviewing your paycheck in MOLI.
- When submitting the form, focus only on incremental (additional) amounts of hours to be paid for and not the total number of hours worked.
- If an employee is unable to submit an adjustment form, their leader can submit on their behalf.
Thank you for continued patience while we navigate this outage together. For more information, visit our Connect Resources site.
Jeff Wagner
Administrator on Call
Michelle Riley-Brown
EVP on Call
Sunday, December 26, 2021: 4:48 p.m.
Kronos Outage Update: Approval deadline tomorrow at 10 a.m.
Texas Children’s Team Members,
With the close of our latest pay period over the weekend, leaders now have until 10 a.m. tomorrow to approve their employees’ time in Connect Clock. This includes clock in/out times, time off and any applicable pay programs. After this deadline, there will be no more opportunities to make changes prior the issuance of this week’s paycheck, which will be taking place on our normal schedule.
For more information on this process, please see below.
- Check your hours before the deadline. Last week, Texas Children’s IS team released a new View My Time feature within Connect Clock that allows employees to see their punches for the current pay period. Please use this new function to look over your times according to your manual tracking sheet, and if you identify an error, please work with your leader prior to the 10 a.m. Monday deadline to correct any discrepancies.
- Holiday Pay. Thank you to all of our employees who worked over the recent holiday. Please note that due to the Kronos outage, our Payroll team will be adding holiday pay to your upcoming check through a different process. As a result, holiday pay will not appear on your time card in Connect Clock; however, the special pay will appear on your upcoming paycheck. In addition, the holiday pay code will be available on the adjustment form in the event any time needs to be corrected.
- Adjustment Period for Upcoming Check. Although we are striving to minimize errors, this will be our first pay cycle using Connect Clock. As a result, some employees may require corrections to their checks. To capture and compensate for these adjustments as quickly as possible, Texas Children’s will be processing a special off-cycle pay distribution for Jan. 6, though when funds will be received is dependent on the employee’s banking institution.
In order to be included in this distribution, employees must submit any corrections via a Timekeeping Adjustment Form – and have it approved by their leader – no later than 10 a.m. on Jan. 3. Please review your pay slip in MOLI later this week prior to submitting an adjustment form for the most recent pay period.
Thank you for your agility and patience as we continue to work through solutions together. More information will be communicated as we head into the week.
Ketrese White
Administrator on Call
Dan DiPrisco
EVP on Call
Thursday, December 23, 2021: 5:11 p.m.
Kronos Outage Update: New Connect Clock functionality
Texas Children’s Team Members,
As we continue to update our tools during the ongoing Kronos outage, our Information Services team has launched two new features today for Connect Clock. Please see updates below.
- Connect Clock Best Practices. To ensure accurate timekeeping, please review this brief list of best practices for accessing Connect Clock and entering time (for leaders).
- For non-exempt (hourly) employees: A new View My Time feature has been added, which allows employees to see their punches for the current pay period after verifying their identity. Please use this new function to look over your times according to your manual tracking sheet. If you identify an error, please work with your leader to correct any discrepancies.
- For leaders: Managers now have the ability to delete punches. Please note that once time is approved, managers will not be able to make changes, so ensure accuracy of all punches for each day prior to approving. Time should also be inputted in standard time – not military time. Additionally, do not use leading zeros when entering time. For example, 08:30 should be entered as 8:30.
As of today, all hours from Dec. 12 – Dec. 17 should be entered into the Connect Clock system. As was previously our process, hours, time off, and special pay codes for the pay period must be reviewed and approved by leaders no later than 10 a.m. Monday, Dec. 27.
Thank you for your agility and patience as we continue to work through solutions together. More information will be communicated as we know more.
Ketrese White
Administrator on Call
Dan DiPrisco
EVP on Call
Sunday, December 19, 2021: 9:40 p.m.
Kronos Outage Update: Connect Clock User Guide and Guidance on Punches
Texas Children’s Team Members,
As we continue to navigate the timekeeping challenges from the Kronos outage, we wanted to provide you with a few updates related to Connect Clock, our new time tracking tool for hourly employees, as well as what to do with your manual tracking sheets. Please see below for additional guidance.
- Connect Clock User Guide. To access a step-by-step user guide with visuals on where to find Connect Clock and how to use it, please click here.
- Guidance on Punches for Meal Breaks. At this time, Connect Clock only allows for up to four punches per shift, including clocking in and out for meal breaks. If your shift requires multiple meal breaks, please track any additional meal breaks greater than 20 minutes on the manual tracker form and notify your leader. However, you are not required to clock out for any second meal breaks in Connect Clock at this time.
- Manual Tracker Sheets. As a reminder, hourly employees are asked to please photocopy or take a picture of your timekeeping sheet (for personal records) and then submit the original to your leader. Additionally, while we validate our new timekeeping tools, please continue to track your time and time off manually using the tracking sheet to ensure all hours are being captured and accurately recorded.
For additional information, please reference this FAQ, which will be continuously updated as we learn more about this situation.
Need Help? As an employee resource during this event, Texas Children’s has initiated an Employee Support Center, which can be reached by calling 832-826-4700. The line will be open Monday through Friday from 7 a.m. to 5 p.m. You may also email any time at hremployeesupportcenter@texaschildrens.org.
Thank you for your efforts. We wish you a good holiday week, and we will be in touch as we have more information about our response.
Janet Winebar
Administrator on Call
Mark Mullarkey
EVP on Call
Sunday, December 19, 2021: 8 a.m.
Kronos Outage Update: Timekeeping Adjustment Form due tomorrow at 10 a.m.
Texas Children’s Team Members,
As a reminder, tomorrow at 10 a.m. is the deadline to submit a Timekeeping Adjustment form to report any underpayments in your most recent paycheck prior to a special off-cycle pay run Texas Children’s will be making on Dec. 22. Any forms received after this time will be processed as quickly as possible, along with any other adjustments that must be made as a result of the Kronos outage.
- Please note that this form requires leader approval.
- Leaders are asked to monitor their email to review and approve submissions prior to the deadline. To better inform the approval of adjustment requests, access this dashboard to view the hours of direct reports in accordance to our payroll system.
- When submitting adjustments, please reference hours paid on the Dec. 16 paycheck, which is available in MOLI.
- Focus only on incremental (additional) amounts of hours to be paid for and not the total number of hours worked.
- If an employee is unable to submit an adjustment form, their leader can submit on their behalf.
Texas Children’s commits to paying our employees on time and to review and correct any underpayments as quickly as possible. We appreciate your patience while we navigate this situation together.
Questions? For additional information, please reference this FAQ, which will be continuously updated as we learn more about this situation.
Need Help? As an employee resource during this event, Texas Children’s has initiated an Employee Support Center, which can be reached by calling 832-826-4700. The line will be open Monday through Friday from 7 a.m. to 5 p.m. You may also email any time at hremployeesupportcenter@texaschildrens.org.
Thank you for your efforts.
Janet Winebar
Administrator on Call
Mark Mullarkey
EVP on Call
Friday, December 17, 2021: 5:40 p.m.
Kronos Outage Update: Introducing Connect Clock for Hourly Employees
Texas Children’s Team Members,
In response to the Kronos outage, our IS team has worked diligently to launch Connect Clock, a timekeeping tool available on the Connect homepage for all hourly employees. This time clock is available today for employees beginning their shifts at 6 p.m. or after. If you began a shift before this time, please use the manual tracker sheet to clock out and begin using Connect Clock on your next shift. We will transition to this new process over the next 24 hours to give our team members time to adjust. Please do not clock in or out with the Kronos time clocks as they are not currently functioning.
- How to Use Connect Clock. At the start of your shift, log in to a Texas Children’s computer or Texas Children’s network using your username and password and follow these instructions.
-
- Go to the Connect homepage and click the banner titled “Connect Clock”
- Follow the steps to verify your identity and to clock in or out (including for meal breaks)
- When using a shared computer, log out once you are finished so other employees can log in using their credentials
- Manager Timekeeping Tool. Our team is developing an online manager timekeeping tool where leaders can review time, enter pay codes and other functions. It’s expected to launch in the next few days, and we will provide more information soon.
- Manual Tracker Sheets. Along with the manager timekeeping tool, there will be a solution for entering time that has already been captured by the manual tracking sheets for this pay period. For now, hourly employees are asked to please photocopy or take a picture of your timekeeping sheet (for personal records) and then submit the original to your leader, who is being asked to aggregate all tracking sheets for their teams. More information on this timekeeping process for manual tracking sheets will be coming as soon as possible. Additionally, while we validate our new timekeeping tools, please continue to track your time and time off manually using the tracking sheet to ensure all hours are being captured and accurately recorded.
For additional information, please reference this FAQ, which will be continuously updated as we learn more about this situation. As always, please also consult your leader on any guidance related to this incident.
Thank you for your patience as we work through this incident. More information will be communicated throughout this event.
Janet Winebar
Administrator on Call
Mark Mullarkey
EVP on Call
Thursday, December 16, 2021: 8:30 p.m.
Kronos Outage Update: New Timekeeping Adjustment Form
Texas Children’s Team Members,
Throughout the week, our teams have been working hard to respond to the Kronos outage, and we truly appreciate your patience while we do everything we can to ensure that pay is on time and accurate, and to correct underpayments as quickly as possible. Please see below for updates on a new Timekeeping Adjustment Form, which must be submitted to correct any missed hours from the most recent paycheck.
- **New** Timekeeping Adjustment Form. As communicated yesterday evening, if an employee sees a discrepancy in their most recent paycheck, we ask that you please submit a new Timekeeping Adjustment form by 10 a.m. Monday, Dec. 20 (please note that this form requires leader approval).
If you previously submitted a Timekeeping Adjustment, we ask that you resubmit using this new form. We again apologize for any inconvenience. This new form has been updated to better accommodate the types of adjustments our employees will need to submit during this event and will help expedite the process moving forward.
When submitting any adjustments, please reference hours paid on the Dec. 16 paycheck, which is available in MOLI. Additionally, adjustment forms should focus only on incremental (additional) amounts of hours an employee needs to be paid for, and not the total number of hours worked. If are unable to submit an adjustment form, please work with your leader to have a form submitted on your behalf.
Once approved, Texas Children’s will process a special pay cycle for Wednesday, Dec. 22, although when the funds appear in the employee’s account will be determined by their bank. In order for your adjustment to be included in this pay cycle, a new adjustment form must be submitted to and approved by your leader before 10 a.m. Monday, Dec. 20. Forms received after this time will be processed in the next pay cycle the following week.
When tracking hours for the CURRENT pay period, employees and leaders should continue using the manual spreadsheet until further notice.
- Pay codes. Given the number of pay code options Texas Children’s uses, the adjustment form does not currently capture all pay programs. However, if an employee simply needs to report additional hours worked, these hours should be coded as “Reg.” From there, our payroll team will calculate any overtime that needs to be paid. If an employee needs to apply a specific pay code for their hours – and that code is not listed on the form – we ask that they reference this document to identify codes that have a similar pay structure and are available within the form.
- Employee Support Center. To answer and help resolve questions during this incident, Texas Children’s has initiated an Employee Support Center, which can be reached by calling 832-826-4700. The line will be open Monday through Friday beginning Dec. 14 from 7 a.m. to 5 p.m. You may also email any time at hremployeesupportcenter@texaschildrens.org.
For additional information, please reference this FAQ, which will be continuously updated as we learn more about this situation. As always, please also consult your leader on any guidance related to this incident.
Thank you for your patience as we work through this incident. More information will be communicated throughout this event.
Janet Winebar
Administrator on Call
Mark Mullarkey
EVP on Call
Wednesday, December 15, 2021: 6:45 p.m.
Kronos Outage Update
Texas Children’s Team Members,
Thank you for everyone’s patience and partnership as we work through the impacts of the ongoing Kronos outage. To update on Monday’s global message, please see below for the latest information related to this event.
- Data Breach. One question our employees have asked is what information from Texas Children’s may have potentially been accessed as a result of this breach. Although the investigation into this event is still ongoing, we can confirm that Texas Children’s shares limited information through Kronos, which does not include social security numbers, employee banking information or pay rates. We will continue to work closely with Kronos to learn more about this breach.
- **New** Timekeeping Adjustment Form. As communicated Monday, Texas Children’s will reference the pay period ending Nov. 13 to populate hours worked for the coming paycheck. Although we selected this time period to best represent a normal work week, and did our best to limit underpayments, we understand some employees will be underpaid. If you see a discrepancy in your upcoming paycheck, you will be asked to submit a Timekeeping Adjustment form by 10 a.m. Monday, Dec. 20 (please note that this form requires leader approval).
Following previous communications, our payroll team received multiple submissions of our Timekeeping Adjustment Form, many of which were cancellation requests for previous submissions that had been made prior to payroll being completed. As a result, we are quickly working to make enhancements to our existing Timekeeping Adjustment Form to better accommodate the adjustments being requested. This new form is currently being built and will be made available as quickly as possible.
Please note that if you previously submitted a Timekeeping Adjustment form, you will be asked to resubmit using the new form. We apologize for any inconvenience as we work through the best way to manage these submissions. We remain committed to getting any underpayments resolved as quickly as possible. When submitting any adjustments, please reference hours paid on this Thursday’s paycheck, which is currently available in MOLI. Additionally, adjustment forms should focus only on incremental (additional) amounts of hours an employee needs to be paid for, and not the total number of hours worked.
Once approved, Texas Children’s will process a special pay cycle for Wednesday, Dec. 22, although when the funds appear in the employee’s account will be determined by their bank. In order for your adjustment to be included in this pay cycle, a new adjustment form must be submitted to and approved by your leader before 10 a.m. Monday, Dec. 20.
- Employee Assistance Program (EAP). If you have been negatively impacted by this event, the EAP is also available to you. Please click here to visit the page on Connect to learn more.
- Employee Support Center. To answer and help resolve questions during this incident, Texas Children’s has initiated an Employee Support Center, which can be reached by calling 832-826-4700. The line will be open Monday through Friday beginning Dec. 14 from 7 a.m. to 5 p.m.
For additional information, please reference this FAQ, which will be continuously updated as we learn more about this situation. As always, please also consult your leader on any guidance related to this incident.
Thank you for your patience as we work through this incident. More information will be communicated throughout this event.
Janet Winebar
Administrator on Call
Mark Mullarkey
EVP on Call
Monday, December 13, 2021: 9:24 p.m.
Kronos Update: Downtime Procedure
Texas Children’s Team Members,
Throughout the day, we have been working diligently to respond to the Kronos outage, which has impacted Texas Children’s and many other organizations nationwide. At this time, we do not know when Kronos services will be restored and Texas Children’s will remain disconnected from their systems until we are confident this breach has been safely resolved.
In the meantime, thank you for your partnership in following our downtime procedures and tracking your time manually. Please see below for the latest information on our plans for our current payroll cycle, as well as what employees should do now to ensure proper timekeeping.
- Current Payroll. Given the current pay period recently ended – and timecards were scheduled to be approved this morning – Texas Children’s was unable to access any time captured in Kronos for the pay period ending Dec. 11, including both worked time and paid time off.
To ensure our team members continue to be compensated during this pay cycle, we will be paying employees for hours worked during the pay period ending Nov. 13, including any overtime, shift differential or special pay worked during that period. To calculate pay, we will reference rates as of Dec. 11.
While we understand some employees will be compensated for more or less than what they actually worked this last pay period, we determined this was the best option to get as close as possible to what employees can expect. If an employee is underpaid for the pay period ending Dec. 11, the employee is asked to submit a Timekeeping Adjustment Form by 10 a.m. Monday, Dec. 20. Upon receiving this form, Texas Children’s will process a special pay cycle for Wednesday, Dec. 22, although when the funds appear in the employee’s account will be determined by their bank.
For additional information and other scenarios, please reference this FAQ, which will be continuously updated as we learn more about this situation.
- Merit increases. All merit increases set to take effect prior to Dec. 11 will be used to calculate pay amounts for the upcoming check.
- New employees. For new employees that did not work during the pay period ending Nov. 13, we will pay standard hours based on their start date.
- Timekeeping for hourly employees. As a reminder, until further notice, we ask that all our non-exempt (hourly) employees transition to managing their time manually using the tracker form. Please record all time that you have worked starting Saturday, Dec. 11 at 12 a.m. Salaried employees will be compensated according to their standard hours and should only use this form for tracking time off.
- PTO/EIB hours. For any PTO or EIB hours not already submitted into Kronos, please input these hours manually using the tracker form and then submit to your leader for review at the end of your final shift before Saturday, Dec. 25.
- Benefits. Given our benefits programs work on a separate system – and not Kronos – we do not anticipate impacts to benefits deductions. We will communicate any changes as we learn more.
- Employee Support Center. To answer and help resolve employee questions, Texas Children’s has initiated an Employee Support Center, which can be reached by calling 832-826-4700. The line will be open Monday through Friday beginning Dec. 14 from 7 a.m. to 5 p.m.
More information will be communicated as it becomes available. To sign up for emergency text alerts, please follow these instructions.
Thank you for your patience as we work through this incident. We continue to appreciate your resiliency and everything you do as One Amazing Team.
Shannon Zerber
Administrator on Call
Mark Mullarkey
EVP on Call
Monday, December 13, 2021: 3:16 p.m.
Incident Command Initiated for Kronos Outage
Texas Children’s Team Members,
To follow-up on the global communication from Information Services yesterday, Texas Children’s is currently being affected by a Kronos outage that began late Saturday and is impacting many organizations nationwide.
As of this morning, we have learned that this incident is due to a ransomware attack on Kronos’ systems. Texas Children’s was able to disable our connection with their systems yesterday, and we will remain disconnected until we are confident this breach has been safely resolved by Kronos and services fully restored.
Additional communications about this incident – as well as a full set of FAQ – will be distributed shortly. In the meantime, please know the following:
Updates
- Incident Command. Effective immediately, Texas Children’s has stood up its Incident Command for this Kronos outage and will also be enabling its processes for manual timekeeping.
- Payroll. As you are aware, this week is a pay week for Texas Children’s. We are working through our process, but please be assured that we will pay our workforce on time.
- Tracking time. Effective immediately, for hourly employees who clock in and out, please use the updated manual tracker – available for download here – to track your time. Although our time clocks are currently functioning, given the duration of this event we will need to transition to a manual process for monitoring time immediately. Please record all time that you have worked since the beginning of this pay period, which began at 12 a.m. on Sunday, Dec. 12. For salaried employees, please use this tracker to monitor any paid time off; however, you are not required to use this tracker for hours worked.
- Communication. More information on this event will be communicated as it becomes available. In the meantime, stay tuned for more information through Connect, email and your leader. To sign up for emergency text alerts, please follow these instructions.
Thank you for your patience as we work through this incident. We continue to appreciate your resiliency and everything you do as One Amazing Team.
Shannon Zerber
Administrator on Call
Mark Mullarkey
EVP on Call
Sunday, December 12, 2021: 3:33 p.m.
Kronos Outage Reported
The Kronos website and mobile app are currently unavailable. This issue also impacts multiple non-Texas Children’s Kronos customers. Information Services, Payroll and the vendor are engaged and actively investigating the issue.
While Kronos web is unavailable
During the outage:
- Kronos timeclocks will be available for clocking in and out.
- Kronos timeclocks will be available for functions like requesting time off and editing a missed punch.
- Desktop and mobile app users should manually record hours worked and provide this information to your leader and/or timekeeper.
- Please utilize this linked manual timekeeping template to record time during the outage.
Leader responsibilities
Leaders are responsible for:
- Communicating the process for manually tracking time during the outage to employees
- Ensuring employees’ time is accurately captured
Questions?
If you have questions, please contact the IS Service Desk at ext. 4-3512 (external 832-824-3512).