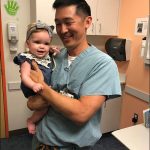
On February 1, Texas Children’s officially welcomed Dr. Brian Smith as the new chief of the Division of Orthopedic Surgery.
“I am delighted that Dr. Smith has joined the Texas Children’s family,” said Surgeon-in-Chief Dr. Larry Hollier. “We believe he will provide seasoned leadership and mentorship for our Orthopedic Surgery faculty and staff.”
As chief of the Division of Orthopedic Surgery, Smith now helms one of the premier pediatric orthopedic surgery programs in the nation, with extensive expertise in the treatment of a variety of conditions, from minor fractures and sports-related injuries, to complex trauma and congenital and developmental disorders.
“I am honored and humbled to join the faculty at one of the very best children’s hospitals and pediatric orthopedic surgery programs in the country,” said Smith. “This division is poised to rise to an even higher level, and I couldn’t be more excited to help it get there.”
Smith joins Texas Children’s from Yale New Haven Children’s Hospital, where he served as Director of Pediatric Orthopedics for the past 11 years and also as Interim Surgeon-in-Chief from 2011 to 2012. Additionally, he served as Yale School of Medicine’s Orthopedic Surgery Residency Director from 2012 to 2018, with 25 residents and rotations at five area institutions.
Smith earned his medical degree and completed his orthopedic residency at Georgetown University School of Medicine before serving four years in the U.S. Air Force as an orthopedic surgeon, where he held the rank of major. He then completed a fellowship in pediatric orthopedic surgery at Boston Children’s Hospital.
Clinically, Smith’s primary interests are spinal deformities and spine surgery. Research interests include spinal deformity in children, maturity indicators in children to assess risk of scoliosis progression, and neuromuscular disorders and fractures.
An active member of the orthopedic professional community, Smith has served on the Board of Directors for the American Academy of Orthopaedics and the orthopedic section of the American Academy of Pediatrics. He has also been health council chair for the Pediatric Orthopaedic Society of North America and chairman of the ethics committee for the Scoliosis Research Society.
In addition to his clinical and research expertise, Smith brings a bright vision of the future for the Division of Orthopedic Surgery.
“My goal is to help us achieve even greater recognition as one of the preeminent destinations nationally and internationally for pediatric orthopedic care,” Smith said. “The opportunity to help this team reach new heights in terms of improving patient care and outcomes, facilitating research, and educating the next generation of pediatric orthopedists is incredible, and I’m looking forward to meeting the challenge.”
Learn more about the Division of Orthopedics and the services we offer.