As we build our bright future Tomorrow, Together, we will continue to offer and improve our best-in-class patient care, service for our members and elite programs for our workforce. We’re already off to an amazing start for the year as the three Texas Children’s Hospital Surgery PA Fellowship Programs become the first and only pediatric-focused programs to receive national accreditation from the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA). Prior to this recognition, there were only seven Clinical Postgraduate PA programs in the U.S. to have received accreditation. What an incredible achievement!
“The PA Fellowship Programs have factored enormously into the growth of our surgical APP program and have raised our profile across the country,” said Dr. Larry Hollier, surgeon-in-chief and chair of the Department of Surgery and medical director for the Surgical PA Fellowship Programs. “These accreditations will certainly make our PA Fellowship Programs some of the most sought-after opportunities for recent graduates and experienced generalists interested in specialization. We are incredibly proud of how this program has evolved over the last decade.”
The newly accredited programs are:
- Texas Children’s Hospital Surgery Physician Assistant Fellowship Program
- Texas Children’s Hospital Orthopedic Physician Assistant Fellowship Program
- Texas Children’s Hospital Community Surgery Physician Assistant Fellowship Program
“These programs are truly one of a kind,” said Jordan Rodriguez, chief administrative officer for the PA Fellowship Program. “It is such an honor to see each class of fellows arrive and grow not only as clinicians but as well-rounded providers. The opportunities they get to experience throughout the year amazes me, and I am so happy we can proudly say we are accredited.”
New applicants can be assured that Texas Children’s provides a well-rounded education program to prepare them with a strong foundation of skills for the future. The programs can accept a combined 10 fellows each year to learn the ins and outs and to work in each surgical subspecialty. It is a unique opportunity that most providers never experience.
“The medical knowledge and interpersonal skills our PA fellows develop during their training becomes invaluable as they progress in their career,” said Kris Marsack, director of Surgery APPs and academic director for the Surgical PA Fellowship Programs.
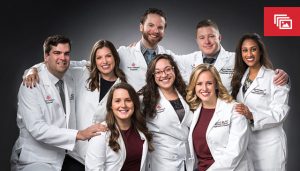
The accreditation could not have been possible without the dedication and tireless efforts of the planning committee who worked for the better part of a year completing applications, planning in person and virtual site visits. Amazing team effort by the accreditation planning committee members below.
- Dr. Larry Hollier, Medical Director
- Kristina Marsack, PA-C, Academic Director
- Ryan Krasnosky, MPAS, PA-C, DFAAPA, DrPH Assistant Director
- Jackie Broda, PA-C, Program Director
- Jordan Rodriguez, Chief Administrative Officer
- Magda Gonzalez, Program Coordinator