March 20, 2018
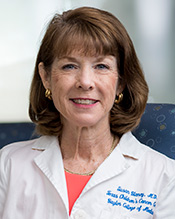
 Dr. Huda Zoghbi, director of the Jan and Dan Duncan Neurological Research Institute at Texas Children’s, Howard Hughes Medical Institute investigator and professor at Baylor College of Medicine, has been awarded the sixth annual Ross Prize in Molecular Medicine by The Feinstein Institute for Medical Research at Northwell Health.
Dr. Huda Zoghbi, director of the Jan and Dan Duncan Neurological Research Institute at Texas Children’s, Howard Hughes Medical Institute investigator and professor at Baylor College of Medicine, has been awarded the sixth annual Ross Prize in Molecular Medicine by The Feinstein Institute for Medical Research at Northwell Health.
The Ross Prize is awarded annually by Molecular Medicine to scientists who have made a demonstrable impact in the understanding of human diseases pathogenesis and/or treatment, and who hold significant promise for making even greater contributions to the general field of molecular medicine.
“It is an honor to be recognized by Molecular Medicine and to join the prestigious roster of past Ross Prize recipients,” said Zoghbi, professor in the Departments of Pediatrics, Molecular and Human Genetics, Neurology and Neuroscience at Baylor. “I look forward to discussing my work and furthering a dialog that I hope will encourage young trainees to join the fields of neurobiology and molecular medicine.”
The prize, which includes a $50,000 award, will be presented to Zoghbi on June 5 at the New York Academy of Sciences in New York City, followed by lectures from Zoghbi and other eminent researchers. The Ross Prize is awarded through the Feinstein Institute’s peer-reviewed, open-access journal, Molecular Medicine, and made possible by the generosity of Feinstein Institute board members Robin and Jack Ross.
“Huda Zoghbi’s examination of the genetic causes for neurological diseases, such as spinocerebellar ataxia and Rett syndrome, has led to a better understanding of neurobiology,” said Feinstein Institute President and Chief Executive Officer Dr. Kevin J. Tracey, who also serves as editor emeritus of Molecular Medicine. “It is through her discoveries that researchers are able to identify new, potential therapies for these conditions that currently have no cure.”
Zoghbi’s research focuses on identifying the genetic causes of neurodegenerative and neurodevelopmental diseases and a broader understanding of neurobiology. Her lab, along with Harry Orr’s team at the University of Minnesota, discovered that excessive repeats of the DNA segment, CAG, in the ATAXIN-1 gene causes the neurodegenerative disease spinocerebellar ataxia type 1 (SCA1). Over time, SCA1 may cause mental impairment, numbness, tingling or pain in the arms and legs and uncontrolled muscle tensing, wasting and twitches. Understanding the genetic cause for SCA1 has inspired additional research that may identify a therapeutic strategy for this condition that affects coordination and balance, difficulties with speech and swallowing, and weakeness in the muscles that control eye movement.
Zoghbi’s lab also has identified the genetic mutations that cause Rett syndrome. Rett syndrome mostly targets young girls and is a postnatal neurological disorder which causes problems in diverse brain functions ranging from cognitive, sensory, emotional, and motor to autonomic functions. These can affect learning, speech, sensations, mood, movement, breathing, cardiac function and even chewing, swallowing and digestion. Zoghbi’s discoveries provide a framework for understanding this disorder as well as the MECP2 duplication disorder and for charting a path for potential therapeutic interventions.
 The Clinical Research Center/Research Resources Office presented the Clinical Research Award for Second Quarter 2018 to Debbie Barrera, nurse manager, Research Resources Office (RRO).
The Clinical Research Center/Research Resources Office presented the Clinical Research Award for Second Quarter 2018 to Debbie Barrera, nurse manager, Research Resources Office (RRO).

 The Department of Surgery hosted the ninth annual Edmond T. Gonzales Jr. Surgical Research Day May 18 at Texas Children’s Pavilion for Women providing a forum for researchers across the department to showcase their work.
The Department of Surgery hosted the ninth annual Edmond T. Gonzales Jr. Surgical Research Day May 18 at Texas Children’s Pavilion for Women providing a forum for researchers across the department to showcase their work.















 The Society for Pediatric Research (SPR) recently gave two Texas Children’s trainees national research awards for their outstanding research on kidney disease at this year’s annual Pediatric Academic Societies’ SPR meeting.
The Society for Pediatric Research (SPR) recently gave two Texas Children’s trainees national research awards for their outstanding research on kidney disease at this year’s annual Pediatric Academic Societies’ SPR meeting.
 Dr. Susan Blaney, deputy director of Texas Children’s Cancer and Hematology Centers, recently received a Director’s Service Award from the National Cancer Institute for her outstanding and dedicated service to the Institute and the Clinical Trials and Translational Research Advisory Committee from 2015 to 2017.
Dr. Susan Blaney, deputy director of Texas Children’s Cancer and Hematology Centers, recently received a Director’s Service Award from the National Cancer Institute for her outstanding and dedicated service to the Institute and the Clinical Trials and Translational Research Advisory Committee from 2015 to 2017. Dr. Huda Zoghbi, director of the Jan and Dan Duncan Neurological Research Institute at Texas Children’s, Howard Hughes Medical Institute investigator and professor at Baylor College of Medicine, has been awarded the sixth annual Ross Prize in Molecular Medicine by The Feinstein Institute for Medical Research at Northwell Health.
Dr. Huda Zoghbi, director of the Jan and Dan Duncan Neurological Research Institute at Texas Children’s, Howard Hughes Medical Institute investigator and professor at Baylor College of Medicine, has been awarded the sixth annual Ross Prize in Molecular Medicine by The Feinstein Institute for Medical Research at Northwell Health.