June 12, 2018
 As Texas Children’s continues to expand its physical footprint as a leader in pediatric care, Texas Children’s Neurology Program is growing by leaps and bounds. As one of the largest pediatric neurology service providers in the nation, more than 30,000 patient encounters occur each year at Texas Children’s Neuroscience Center.
As Texas Children’s continues to expand its physical footprint as a leader in pediatric care, Texas Children’s Neurology Program is growing by leaps and bounds. As one of the largest pediatric neurology service providers in the nation, more than 30,000 patient encounters occur each year at Texas Children’s Neuroscience Center.
Ranked No. 4 nationally in neurology and neurosurgery by U.S. News & World Report, patients are treated for a number of neurological conditions in our 13 specialty clinics including epilepsy, cerebral palsy, Rett syndrome, Batten disease and movement disorders. Many patient families are referred to Texas Children’s for our integrated expertise and multidisciplinary team approach in diagnosing and treating childhood neurological disorders. Recently, the Neurology division expanded its services with the opening of the Angleman Syndrome Clinic to treat children with this very rare, neurogenetic disorder.
“Over the last decade, our neuroscience programs have experienced phenomenal growth,” said Chief of Neurology and Developmental Neuroscience Dr. Gary Clark. “In 2004, the division had 5,000 patient encounters per year. Since then, we have more than quadrupled our patient encounters to 31,500 in 2017. More than half of these patients are seen in the community, allowing for greater access to care.”
In 2017, the neurology service received 1,300 new patient referrals each month which is a 30 percent increase from last year. To meet the increased demand for these services and to accommodate the growing patient population, the pediatric neurology division faculty expanded from 9 to 52 neurologists.
While enhancing access to patient care remains a top priority for Texas Children’s, one way the Neurology service is helping to achieve this collaborative milestone is through the implementation of telemedicine, an interactive telecommunications system that uses real-time video technology to link patients with their primary care and specialty providers. Instead of making the trek to the Texas Medical Center, patients can now “see” their neurologist without ever leaving their primary care clinic.
“Through an HRSA grant, we have seen children with epilepsy in one of our medical homes via this new technology and completed more visits than any other grant recipient,” said Brian Cordasco, practice administrator for Neurology. “This successful experiment will serve as a blueprint for future growth of telemedicine at Texas Children’s. Six faculty offices are now equipped with telemedicine capabilities.”
To balance outpatient services with the increasing demand for inpatient care, the Neurology Service has also developed an inpatient service rotation for physicians at Texas Children’s Hospital West Campus. Just like Texas Children’s Medical Center Campus and Texas Children’s Hospital The Woodlands, neurologists and epileptologists take turns working out of clinic to take neurology consults at the hospital.
Partnerships advance clinical research in neurology
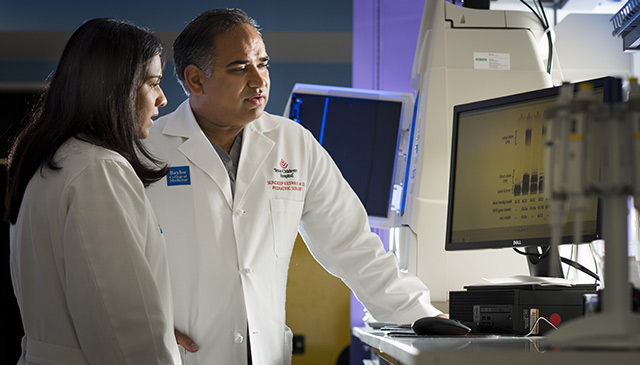
The neurology division’s partnership with the Jan and Dan Duncan Neurological Research Institute (NRI) at Texas Children’s under the leadership of Dr. Huda Zoghbi also has helped to advance clinical and basic science research leading to the development of new treatments for neuro and developmental disabilities.
Nearly $185 million has been raised to build and partially endow the NRI, and the hospital’s long-time philanthropic partner, The Blue Bird Circle, has raised funds (initial gift $1M for four years) to form and partially endow the Blue Bird Circle Clinical Research Center in which NRI discoveries are realized through clinical trials.
The Blue Bird Circle has been the catalyst for so much of what has happened in pediatric neurology in the past 20 years at Texas Children’s. Clinical research protocols have grown from 9 to 63 over the 8-year existence of the Blue Bird Circle CRC. The Blue Bird Circle has raised in excess of $1.2 million annually to directly fund clinical treatment, training and research in pediatric neurology at Texas Children’s.
Through these collaborative research partnerships, the neurology team has made significant progress:
- Texas Children’s is one of the few sites in the country that provides therapy to patients with an enzyme deficiency in the form of Batten disease by surgically injecting the synthesized enzyme directly into the brain thereby halting this degenerative form of Batten disease.
- Texas Children’s treats patients with spinal muscular atrophy, a disease where the spinal cord degenerates due to a defective SMN1 gene. This treatment involves injecting a DNA molecule into the spinal fluid that turns a latent gene into an effective one that makes the deficient protein.
“We are contemplating similar treatments for Angelman and Rhett syndromes,” Clark said. “We are so grateful to Texas Children’s Blue Bird Circle Research Center in collaboration with the Jan and Dan Duncan Neurological Research Institute at Texas Children’s for helping us make these research breakthroughs possible, and I am excited about what the future will hold for pediatric neurology.”



 The Southwest Pediatric Device Consortium (SWPDC), anchored at Texas Children’s Hospital and Baylor College of Medicine, recently received a prestigious P50 grant from the U.S. Food and Drug Administration. The five-year, $6.75 million grant will begin on September 1 and will allow SWPDC to leverage ongoing activities to expand and accelerate the development of much-needed pediatric medical devices. The five principal investigators include Drs. Chester Koh and Henri Justino of Texas Children’s and Baylor, Dr. Balakrishna Haridas of Texas A&M University, Dr. Maria Oden of Rice University, and Dr. Michael Heffernan of Fannin Innovation Studio.
The Southwest Pediatric Device Consortium (SWPDC), anchored at Texas Children’s Hospital and Baylor College of Medicine, recently received a prestigious P50 grant from the U.S. Food and Drug Administration. The five-year, $6.75 million grant will begin on September 1 and will allow SWPDC to leverage ongoing activities to expand and accelerate the development of much-needed pediatric medical devices. The five principal investigators include Drs. Chester Koh and Henri Justino of Texas Children’s and Baylor, Dr. Balakrishna Haridas of Texas A&M University, Dr. Maria Oden of Rice University, and Dr. Michael Heffernan of Fannin Innovation Studio.
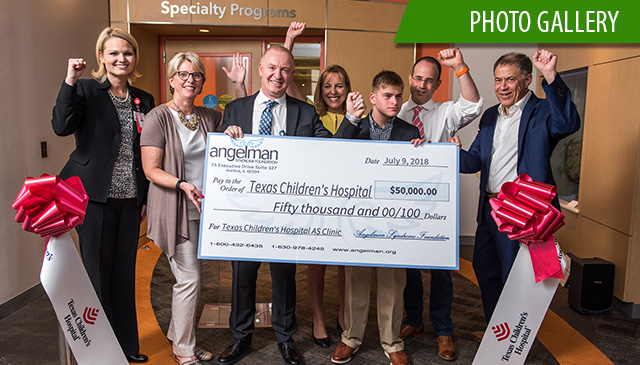 On July 9, Texas Children’s Hospital and the Angelman Syndrome Foundation celebrated the official opening of the Angelman Syndrome Clinic at Texas Children’s, one of only seven Angelman syndrome-specific clinics in the United States – and the first in Texas.
On July 9, Texas Children’s Hospital and the Angelman Syndrome Foundation celebrated the official opening of the Angelman Syndrome Clinic at Texas Children’s, one of only seven Angelman syndrome-specific clinics in the United States – and the first in Texas.















 Scientists at Texas Children’s Hospital, Rice University and Baylor College of Medicine have won a prestigious National Institutes of Health grant to study the dynamic processes and cellular players linked to
Scientists at Texas Children’s Hospital, Rice University and Baylor College of Medicine have won a prestigious National Institutes of Health grant to study the dynamic processes and cellular players linked to  Dr. Zhandong Liu, assistant professor at Baylor College of Medicine and researcher at the Jan and Dan Duncan Neurological Research Institute (NRI) at Texas Children’s has received a distinguished service award from the International Association for Intelligent Biology and Medicine (IAIBM).
Dr. Zhandong Liu, assistant professor at Baylor College of Medicine and researcher at the Jan and Dan Duncan Neurological Research Institute (NRI) at Texas Children’s has received a distinguished service award from the International Association for Intelligent Biology and Medicine (IAIBM). As Texas Children’s continues to expand its physical footprint as a leader in pediatric care, Texas Children’s Neurology Program is growing by leaps and bounds. As one of the largest pediatric neurology service providers in the nation, more than 30,000 patient encounters occur each year at Texas Children’s Neuroscience Center.
As Texas Children’s continues to expand its physical footprint as a leader in pediatric care, Texas Children’s Neurology Program is growing by leaps and bounds. As one of the largest pediatric neurology service providers in the nation, more than 30,000 patient encounters occur each year at Texas Children’s Neuroscience Center.