The Sickle Cell Program at Texas Children’s Hematology Center is the largest in Texas, serving more than 1,000 children a year. The clinic offers the latest treatments for the inherited red blood cell disorder and conducts some of the top research in the field.
The program’s multidisciplinary staff is made up of board-certified pediatric hematologists, hematology-trained nurse practitioners and physician assistants, research staff, as well as social worker and child life specialists. A couple of providers suffer from sickle cell themselves, giving them a unique perspective in caring for their patients.
Texas Children’s Sickle Cell Program Hematologist Dr. Titilope Fasipe and Nurse Practitioner Precious Uwaezuoke both have sickle cell disease. In honor of National Sickle Cell Disease Awareness Month, we talked to them about why they chose to dedicate their profession to caring for children with sickle cell disease and whether living with the disease has allowed them to better connect with patients and their family members.
How has sickle cell affected your life?
Uwaezuoke: My journey with sickle cell has been a tough one. I was in and out of the hospital multiple times when I was younger and there were occasions when I would get depressed. Thanks to family and staff here at Texas Children’s Sickle Cell Program, I was encouraged to stay the course. Sickle cell flares still occur, but I’m able to manage my disease by living a healthy lifestyle and hydroxyurea therapy.
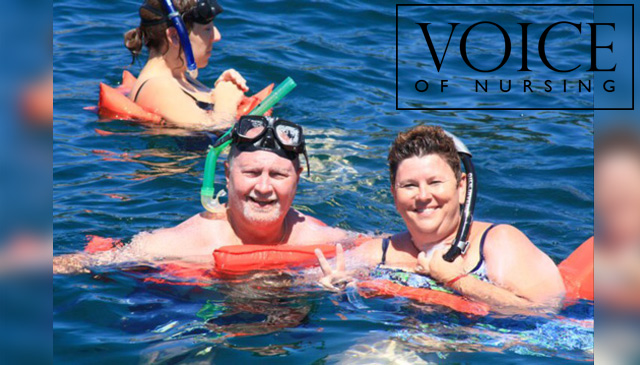
Fasipe: I too suffered from bouts of depression during my early years of battling sickle cell disease. One of my lowest points was when my cousin died from the disease at just 17 years old. Childhood deaths related to sickle cell are not uncommon in Nigeria, which is where I’m from and where screenings and treatments are limited. Because of this, I try not to take life for granted and believe in treasuring all moments, big and small. Like Precious, hydroxyurea has also made a positive difference in my life.
Why did you decide to get into the medical field and help people like yourself?
Uwaezuoke: The treatment I received and the people I met at Texas Children’s inspired me to go into the medical field and help people like myself. I will never forget a nurse who told me to not let sickle cell take over my life; that I could and would be able to do more than just deal with my disease. The connection she made with me during that hard stay in the hospital is part of what made me pursue what is now my passion.
Fasipe: My cousin’s death and my parents’ encouragement motivated me to make a difference in the world and to do work that would help prevent any more deaths like hers. I chose pediatric hematology because I wanted to reach sickle cell patients and their families before they defined how their lives are going to be; and teach them that life can still be beautiful with this disease.
How has having sickle cell helped you connect with patients and families?
Uwaezuoke: A lot of people are devastated when they find out their child has sickle cell disease. Some think it’s a death sentence. The minute I tell them I have the disease and have managed to live a productive, well-balanced life, they break down in tears. They are overjoyed to meet someone older who is living with and managing their disease.
Fasipe: I think many of the families think I can read their minds! For the parents, I acknowledge the guilt and worry they have; and for the children, I acknowledge their pain and fears. After discussing the challenges, we then talk about how we can work together to best manage their disease. The bravery I have seen in our patients has inspired me to become a community sickle cell advocate. I have participated in several Houston sickle cell programs, and served on the first Sickle Cell Advisory Committee of the Texas Department of State Health Services. Precious and I also help coordinate the Texas Children’s Hematology Center’s annual Sickle Cell Education and Research Day, which was recently held at the Houston Museum of Natural Science.
How much progress is being made in finding better treatments cures, for sickle cell disease?
Uwaezuoke: I’m very optimistic. Funding for sickle cell research continues to grow as well as the number of people trying to find better ways to help people with the disease. People who have sickle cell are living longer, especially here in the United States where newborns are screened. All of these things are a step in the right direction.
Fasipe: We are learning more about this disease every day. There are currently several disease-modifying treatments in various stages of the research pipeline; some with successful clinical trials. Gene therapy trials have also shown promise to be a more universal cure than bone marrow transplant, which is only available to a few patients. I am encouraged by how far things have come since I was a child. And, I believe things will only get better.
To learn more about The Sickle Cell Program at Texas Children’s Hematology Center, click here.