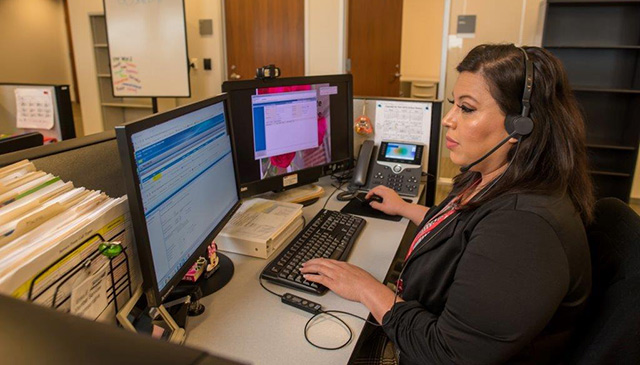
In less than a year, the Member Services team at Texas Children’s Health Plan has completely transformed the way they work, the way they win, and the way they are regarded across the system. A true Cinderella story.
Once known for struggling to meet performance expectations, Member Services now shines in team spirit, employee performance, and the delivery of services to members and providers.
April 2020 marked the most successful performance month for the department in over four years – an accomplishment that is beyond remarkable considering the changes they’ve faced during the current global pandemic.
A comparison of May 2019 and April 2020 demonstrates a number of key accomplishments including but not limited to an increased answer rate of 19 percent, decreased abandonment rate of 7 percent, and a decreased rollover rate of 22 percent to our back up vendor.
“I am so proud of my team and what we have been able to accomplish together. Most importantly, I am especially pleased that our improvements are having a positive impact on the members and providers that depend on us,” said Opera Wagner-Ross, director of Member Services.
Wagner-Ross, who joined the Health Plan in May of 2019, is the undeniable linchpin who has made this transformation possible; however, she doesn’t see it that way. She readily credits her team and the incredible leadership she has received from Richelle Fleischer, senior vice president; and Mark Mullarkey, president of Texas Children’s Health Plan and executive vice president of Texas Children’s Hospital.
“Even the best leaders benefit from good leadership,” she said. I feel incredibly lucky to have the opportunity to work with both Richelle and Mark. They are both dynamic leaders with high expectations. I have learned a great deal over the past year and feel lucky to be a part of the team.” Wagner-Ross went on to say that having great coworkers and a friendly dose of competiveness is also a great motivator. She credits the Claims department at the Health Plan as being an inspiration and a motivator.
“April Riggs, director of Claims, and her team have been very successful in turning things around in the Claims Department. She has been a great partner in that she challenges me, holds me accountable, and can be counted on to make me laugh when faced with challenging situations. She’s the best!”
So how did they do it? How exactly did they spark this kind of change within the department?
Here are the major keys:
- A defined career path for members of the team. By creating a clear career path, employees understood what their options were for growth. With increased opportunity for growth, department retention improved.
- An increase in the number of Spanish speaking agents. A large percentage of health plan members speak Spanish; however only 16 percent of our agents spoke the language. Today, that number sits at 46 percent.
- Appropriate span of control for managers. With a more appropriate span of control, managers are now able to provide better support, coaching and accountability to their teams.
- Improvement in the training of employees. Staff members received an increased amount of training including a special course taught by the Patient Experience staff, which specifically focused on customer service.
- Allowing data to drive change. Whether it was a process to improve, a system to introduce or a technology to enhance, all decisions were made based on information.
- Improvement in the quality of all phone calls. Increased quality review and monitoring of phone calls and improved handling of escalations with a focus on customer satisfaction.
- Celebrating the small wins. The team looks for every reason to celebrate and highlight accomplishments.
Wagner-Ross says that as a leader she really doesn’t have a secret sauce. She simply believes in finding the right people and always looking for opportunities to improve.