A group of more than 30 Texas Children’s pediatric cardiac intensive care medicine experts – including intensivists, nurse practitioners, cardiologists, cardiovascular surgeons and nurses – recently attended the 14th International Meeting of the Pediatric Cardiac Intensive Care Society (PCICS) in Miami, Florida. It was the largest conference in the society’s history, with more than 700 participants from across the nation and around the world.
Texas Children’s presence was felt throughout the event. Not only were we an institutional sponsor, but our cardiac critical care expertise was on display, with our specialists leading or participating in 40 programs, meetings, research presentations and pro/con debates, which covered a variety of clinical topics, including:
- Simulation and quality improvement
- Managing cardiac arrest
- Bedside rounds
- Ethics and social media
- Approaches to single ventricle neonate management
- Effective communication and counseling
- CICU monitoring
- VAD management
- Healthy work environments
- Global perspectives on CICU education
“As an educational opportunity, this event is extremely important for our people, as it highlights important new research, training initiatives and innovations for patients,” said Dr. Paul Checchia, Texas Children’s associate chief of Critical Care Medicine and immediate past president of PCICS. “But it also allows Texas Children’s faculty and staff, who are recognized leaders in this field on an international level, to showcase their thought leadership and to educate others.”
PCICS is an international forum with more than 1,000 members worldwide that promotes excellence in pediatric cardiac intensive care medicine. The annual meeting – the only one of its kind dedicated exclusively to pediatric to pediatric cardiac critical care – plays a large role in the advancement of research and training that has the ability to improve the care of pediatric patients with congenital heart diseases and acquired cardiovascular diseases.
“PCICS is the premier scientific meeting of our field, and Texas Children’s ‘swept the board’ at this year’s meeting,” said Chief of Critical Care Dr. Lara Shekerdemian. “I am particularly proud that all of our clinician groups that included nursing were so strongly represented. This reflects our belief in the importance of collaboration at every level – from clinical care to academic productivity.”
This year’s PCICS conference held additional significance for Texas Children’s as Checchia was honored with the Anthony Chang Lectureship, the only named lecture in the field of pediatric cardiac intensive care medicine. The award is named in honor of Dr. Anthony Chang, who founded PCICS 20 years ago. The Anthony C. Chang Award for Excellence in Pediatric Cardiac Intensive Care recognizes an attending physician who has made exemplary contributions to the field of pediatric cardiac intensive care and to PCICS, and who is making a positive difference in the lives of colleagues, patients and families, as well as in the communities where they live.
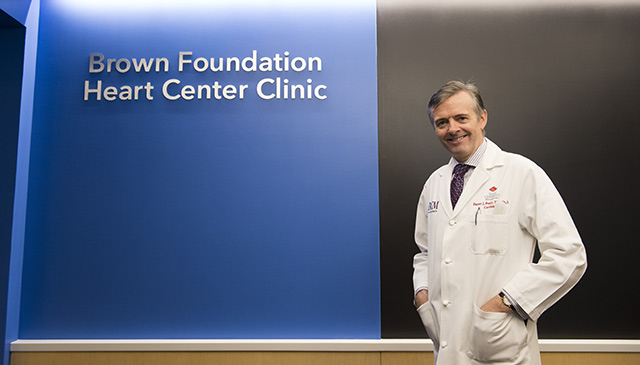
About Texas Children’s Cardiac ICU
Texas Children’s 48-bed CICU is one of the largest and most active units in the nation, and a vital part of the complete continuum of care offered by Texas Children’s Heart Center® – No. 1 in Pediatric Cardiology and Congenital Heart Surgery in the country, according to U.S. News & World Report.
Every year, we admit more than 1,000 children with heart disease, the majority of whom have undergone heart surgery. And we provide comprehensive, specialized care for each child’s individual cardiac condition.
Our multidisciplinary team includes cardiac intensivists, cardiologists, cardiac surgeons, cardiac anesthesiologists, perfusionists, advanced practice providers, nurses and respiratory therapists, all working collaboratively to provide the best care and outcomes for patients. State-of-the-art facilities coupled with dynamic decision-making in the CICU allow our team to carefully analyze each child’s case and deliver a customized care experience. Additionally, we are a recognized leader in cardiac critical care education and are dedicated to training the next generation of specialists and nurses on caring for a patient population with complex needs and interventions.
Learn more about Texas Children’s CICU.