As the opening of the new Heart Center in Legacy Tower quickly approaches, one grateful patient family is commemorating their journey with Texas Children’s with a building project of their own.
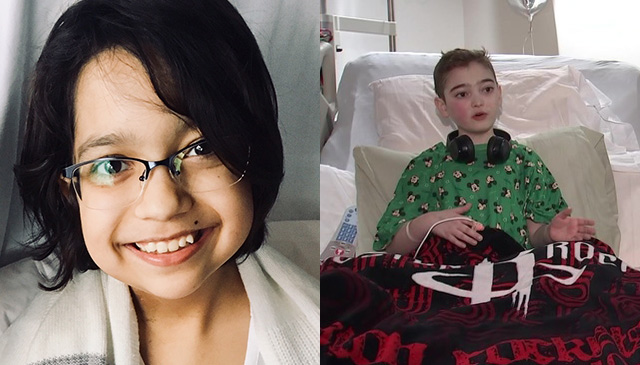
Heartwood Acres is a new subdivision being developed by Rodgers Homes & Construction, a business owned and operated by Jenny and Philip Rodgers, who came to Texas Children’s in 2014 after a routine 20-week ultrasound revealed their baby had hypoplastic left heart syndrome. Their doctors in Shreveport, Louisiana, explained that repairing this rare, complex and life-threatening heart defect would require highly specialized care that wasn’t available locally, including at least three open-heart surgeries, the first just a few days after birth. But even with surgical intervention, survival wasn’t certain. The couple was devastated.
“When they told us something was wrong, everything changed,” Jenny recalled. “I cried for months. It was as though we were mourning the loss of the family life we’d envisioned.”
After researching fetal cardiology and surgical options at top regional and national hospitals, they decided their best chance was treatment at Texas Children’s. From the moment they walked in, they knew they’d made the right choice.
“We were immediately blown away by the facilities and how state-of-the-art everything was, but what really floored us were the people,” Jenny said. “Everyone was incredible and comforting. Dr. Nancy Ayres, our fetal cardiologist, met us in the hallway and stayed with us all day. We felt like we were being taken care of from day one.”
Prior to delivery, Jenny moved to Houston to be closer to Texas Children’s, where she would remain until after her baby’s second open-heart surgery. On May 19, 2014, after months of careful planning and monitoring at Texas Children’s Fetal Center®, Jenny gave birth to Aiden at Texas Children’s Pavilion for Women. Just four days later, Dr. Jeffrey Heinle, associate chief of Congenital Heart Surgery, performed the first of Aiden’s surgeries at Texas Children’s Heart Center®. The family stayed in Houston until Aiden was ready for his second surgery, performed when he was only four months old. Less than a month later, they were discharged to return home to Louisiana.
Today, Aiden is a happy four-year-old who loves superheroes and playing soccer. And though there’s another procedure on the horizon, part of Aiden’s three-stage palliative surgical path, Jenny knows her son and family will be in the best hands possible at the No. 1 heart center in the country according to the 2018-2019 U.S. News & World Report hospital rankings.
“Heart parents are fiercely proud of their heart centers,” Jenny said, laughing. “So we’re excited that ours is the actual No. 1 heart center, especially because the rankings are so comprehensive. That kind of transparency is vital for families that need to make important health decisions. The U.S. News rankings are an easy-to-understand resource that I give to any family I meet that’s in need of specialized care.”
Of added comfort to the Rodgers family is the fact that when Aiden undergoes his final surgery, it will be in the new Heart Center in Legacy Tower. The Heart Center will occupy eight floors and will feature four cardiac catheterization labs including integrated MRI scanner, four cardiovascular operating rooms, three cardiovascular ICU floors with 48 private rooms, two cardiac acute care floors with 42 private patient rooms, and a dedicated space for families.
“I’m thrilled that we’ll have access to this awesome new facility,” Jenny said. “It’s huge to know that because of the layout of the new CVICU rooms, I don’t have to leave to sleep or shower. I can be right where I’m supposed to be – with Aiden.”
The road has been long and their journey isn’t over, but the Rodgers family is grateful for Texas Children’s and the care they’ve received. In honor of their experience, and their continued involvement in the pediatric heart community, the family decided to name their company’s first ever subdivision Heartwood Acres. When residents and visitors pass into the neighborhood, they’ll pass a plaque that tells Aiden’s story and how this place and its streets got their names. The first three streets are appropriately named Fannin, after the street where Texas Children’s stands, Ayres Circle and Heinle Way.
On September 6, the Rodgers family presented Drs. Ayres and Heinle with their own street signs, each with a personal inscription to the people who Jenny said held Aiden’s life – and his heart – in their hands.
The inscription reads:
Your care lit the path for our son Aiden’s life and we are honored to pave the streets in your name for others to live theirs.
“We wouldn’t have Aiden without them,” Jenny said. “They mean so much to us and we love them.”
Learn more of the Rodgers family’s story.




 Texas Children’s Hospital was back on Capitol Hill in June in support of the Children’s Hospital Association Speak Now For Kids Family Advocacy Day, which brings patient families from around the United States to Washington, D.C. to share their experiences with lawmakers and staff, as well as to advocate for policies that will ensure the highest levels of medical care for children and their families.
Texas Children’s Hospital was back on Capitol Hill in June in support of the Children’s Hospital Association Speak Now For Kids Family Advocacy Day, which brings patient families from around the United States to Washington, D.C. to share their experiences with lawmakers and staff, as well as to advocate for policies that will ensure the highest levels of medical care for children and their families. Two congenital heart surgeons will be joining the Texas Children’s Heart Center® team this fall. Dr. Christopher Caldarone will serve as the chief of congenital heart surgery and Dr. E. Dean McKenzie will serve as a congenital heart surgeon.
Two congenital heart surgeons will be joining the Texas Children’s Heart Center® team this fall. Dr. Christopher Caldarone will serve as the chief of congenital heart surgery and Dr. E. Dean McKenzie will serve as a congenital heart surgeon.


















