Bench and Bedside is a digest of the previous month’s stories about the clinical and academic activities of our physicians and scientists. We welcome your submissions and feedback.
Bench and Bedside is a digest of the previous month’s stories about the clinical and academic activities of our physicians and scientists. We welcome your submissions and feedback.
February 2
Texas Children’s, Rice University team up to develop new way to repair birth defect
Bioengineers at Texas Children’s Hospital and Rice University have won a National Institutes of Health grant to develop a new generation of patches to repair the damaged hearts of infants. The $1.9 million, 5-year grant will allow Jeffrey Jacot and his team to take the next steps in a long-running drive to improve the survival rates of such infants, many of whom are diagnosed in utero and require surgery soon after birth.
February 2
Department of State Health Services to award Texas Children’s $1 million grant for SIU 
Texas Children’s is set to receive a $1 million grant from the Texas Department of State Health Services (DSHS) to put toward its newly constructed Special Isolation Unit at Texas Children’s Hospital West Campus. The funds, to be delivered during the next five years, will specifically go toward Ebola preparedness activities that bolster employee safety and quality of care.
February 2
Texas Children’s convenes task force, urges employees to educate themselves on Zika
 In light of the multiple confirmed cases of Zika infection in Texas due to foreign travel, Texas Children’s leaders encourage employees, particularly pregnant women, to refrain from traveling to areas where the outbreak is growing and to follow precautionary measures to protect themselves from Zika exposure. Since the mosquito-carrying virus has been known to increase the risk of microcephaly, a neurological fetal birth defect, Texas Children’s recently convened a task force to develop management and research strategies based on screening criteria outlined by the Centers for Disease Control for pregnant women who may have been exposed to the Zika virus.
In light of the multiple confirmed cases of Zika infection in Texas due to foreign travel, Texas Children’s leaders encourage employees, particularly pregnant women, to refrain from traveling to areas where the outbreak is growing and to follow precautionary measures to protect themselves from Zika exposure. Since the mosquito-carrying virus has been known to increase the risk of microcephaly, a neurological fetal birth defect, Texas Children’s recently convened a task force to develop management and research strategies based on screening criteria outlined by the Centers for Disease Control for pregnant women who may have been exposed to the Zika virus.
February 2 Kline: Children deserve access to best care
Many patients have been left scrambling to find a new medical home when a number of insurance companies decided not to provide in-network coverage for many hospitals in the Texas Medical Center, including Texas Children’s Hospital. Physician-in-Chief Dr. Mark W. Kline talks about how all children deserve access to the best care.
February 2
Zoghbi to receive medal for pioneering advancements in neuroscience research
 Dr. Huda Zoghbi, director of the Jan and Dan Duncan Neurological Research Institute at Texas Children’s, will receive the 2016 Jessie Stevenson Kovalenko Medal from the National Academy of Science in April for her achievements in neuroscience, which includes unlocking the genetic and molecular mysteries behind rare neurological disorders.
Dr. Huda Zoghbi, director of the Jan and Dan Duncan Neurological Research Institute at Texas Children’s, will receive the 2016 Jessie Stevenson Kovalenko Medal from the National Academy of Science in April for her achievements in neuroscience, which includes unlocking the genetic and molecular mysteries behind rare neurological disorders.
February 2
Clinical Research Center presents research award to Dr. Anvari
The Clinical Research Center will present the Clinical Research Award for First Quarter 2016 to Dr. Sara Anvari, physician, Allergy and Immunology. Dr. Anvari is a dedicated clinical scientist for the food allergy research trials at Texas Children’s Hospital.
February 9
Three NRI researchers recognized for their contributions to neuroscience research
Drs. Michael Wangler and Shinya Yamamoto recently obtained a research grant from the Simon’s Foundation for Autism Research Initiative (SFARI) to advance their study on autism spectrum disorders. Their study titled, “In vivo functional analysis of autism candidate genes” is one of five projects selected for research funding by the SFARI. Dr. Andrea Ballabio, founder and director of the Telethon Institute of Genetics and Medicine (TIGEM), Italy, professor at Baylor and faculty member at the NRI, has been selected to receive the 2016 Louis-Jeantet Prize for Medicine. He will share this award with biochemist John Diffley, associate research director at the Francis Crick Institute, United Kingdom.
February 16
Study finds premature infants benefit from exclusive human milk-based diet
 A recent Baylor College of Medicine study led by Texas Children’s neonatologist Dr. Amy Hair, and published in the journal Breastfeeding Medicine, found that premature infants weighing less than 1,250 grams at birth showed improved outcomes after being fed a human milk-based diet.
A recent Baylor College of Medicine study led by Texas Children’s neonatologist Dr. Amy Hair, and published in the journal Breastfeeding Medicine, found that premature infants weighing less than 1,250 grams at birth showed improved outcomes after being fed a human milk-based diet.
February 16
Mata twins celebrate one-year anniversary after historic separation 
A year after being separated in a marathon surgery at Texas Children’s Hospital, formerly conjoined twins Knatalye and Adeline Mata are healthy, lively toddlers. Several members of our medical staff involved in the girls’ care got to see how much they have grown and how far they have come during a recent visit to Texas Children’s for their follow-up appointments with pediatric subspecialists monitoring their health and development. Hear some of their reactions and see for yourself how much the girls have progressed.
February 16
Heart Center launches series of educational animated videos 
Featuring an armadillo, a bison and robot-like caregivers called Blings, a series of animated videos created by Texas Children’s Heart Center aims to help educate patients and their families about various heart conditions and treatment options. Six of the videos were unveiled at a February 15 red carpet premier and can be accessed on the Texas Children’s website at http://www.texaschildrens.org/hearteducation.
February 23
CVICU physician performs CPR, saves man’s life during spin class
When Dr. Natasha Afonso clipped in to a bike for a spin class on a recent Thursday evening, she didn’t know the skills she uses each day to treat patients in the CVICU would mean the difference between life and death for a fellow rider. Toward the end of the 45-minute, high-intensity class, Afonso heard 50-year-old Scott Corron collapse and fall off his bicycle. Because he wasn’t breathing and had no pulse, Afonso immediately started CPR, an action that ultimately saved Corron’s life.
February 23
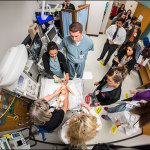
New in situ simulation program enhances role clarity in high-risk emergencies 
Texas Children’s Simulation Center recently launched the first-ever Neonatal Comprehensive In Situ Simulation Program for NICU providers at the Pavilion for Women. The program focuses on improving crisis resource management skills, one of which is role clarity, to ensure all code team members know each other’s specific roles when delivering care to patients during high-risk medical emergencies.
February 23
Texas Children’s helps develop nation’s first hospital-based rapid test for the Zika virus
 Pathologists and clinical laboratory scientists at Texas Children’s Hospital and Houston Methodist Hospital developed the nation’s first hospital-based rapid test for the Zika virus in a matter of weeks as part of the L.E. and Virginia Simmons Collaborative in Virus Detection and Surveillance. Pathologist-in-Chief Dr. James Versalovic and Dr. James Dunn, director of medical microbiology and virology, led Texas Children’s Zika test development team. The new diagnostic test identifies virus-specific RNA sequences to detect the virus and can distinguish Zika virus from other virus infections like Dengue, West Nile or Chikunguny.
Pathologists and clinical laboratory scientists at Texas Children’s Hospital and Houston Methodist Hospital developed the nation’s first hospital-based rapid test for the Zika virus in a matter of weeks as part of the L.E. and Virginia Simmons Collaborative in Virus Detection and Surveillance. Pathologist-in-Chief Dr. James Versalovic and Dr. James Dunn, director of medical microbiology and virology, led Texas Children’s Zika test development team. The new diagnostic test identifies virus-specific RNA sequences to detect the virus and can distinguish Zika virus from other virus infections like Dengue, West Nile or Chikunguny.
February 23
Blaney receives Pioneer Award for contributions in pediatric neuro-oncology The Children’s Brain Tumor Foundation honored Dr. Susan Blaney with the Pioneer Award for Pediatric Neuro-Oncology, celebrating her 25 years of dedication to the search for new and better treatments for children with brain and spinal cord tumors. Blaney’s extensive experience in clinical translational research focuses on developing new treatment strategies for children with brain tumors and other refractory cancers. Blaney has been instrumental in developing more new agent clinical trials than anyone in the field of pediatric oncology.
February 23
Dietrich voted president-elect of North American Society for Pediatric and Adolescent Gynecology
Chief of Pediatric and Adolescent Gynecology Dr. Jennifer Dietrich has been voted president-elect of the North American Society for Pediatric and Adolescent Gynecology. Her tenure as president-elect begins in April. She will be voted in as president in April 2017.
February 23
Texas Children’s Health Plan Center for Children and Women earns accolades for CenteringPregnancy® program Texas Children’s Health Plan’s Center for Children and Women has earned site approval for its CenteringPregnancy® program. The Centering Healthcare Institute (CHI) has awarded both the Southwest and Greenspoint locations the official designation for closely following the CenteringPregnancy® model.