April 22, 2014

Dr. Henri Justino, director of the C.E. Mullins Cardiac Catheterization Laboratory, is something of a magician when it comes to repairing a child’s heart in the least invasive way possible. He and his colleagues in the cath lab can remove a blockage, close a hole in the heart, and replace a defective heart valve using thin, flexible catheters and some deft flicks of the wrist, leaving no trace of their efforts other than a tiny incision near the patient’s hip.
One thing that has consistently bothered him, however, is the lack of available options for children with defective heart valves.
“Compared to the adult market, the pediatric market is simply too small for companies to invest in,” Justino said. “Seventy-five percent of children who need a valve replacement need a pulmonary valve, but there’s only one kind available today that can be delivered by a catheter approach and is approved for use in the pulmonary position. It’s expensive and hard to come by. We need another option.”
Justino and his partners – Daniel Harrington, Ph.D., at Rice University, and Kwonsoo Chun, Ph.D., at Baylor College of Medicine – are on a mission to create an artificial pediatric pulmonary valve that can be delivered by a catheter-based approach into the heart.
“Right now, we are working on getting the mechanics right,” Justino said. “We need a solid valve that works well, opens and closes well with every heartbeat, and is designed to last.”
Getting the valve’s mechanics right is no small feat. It must be small, thin and flexible enough to snake through a young child’s veins and through the chambers of the heart. Once it’s in the right place, it needs to expand to full size, anchor in place with no sutures or adhesive, and be durable enough to last many millions of cycles in a child’s heart, which beats up to twice as fast as an adult’s. They’re also trying to design the valve so that it can grow with a child over time.
“We’ve definitely got some challenges,” said Justino, who compares catheterization to a mechanic trying to fix the motor on a car while it’s still running. “We’re doing all sorts of procedures on the heart without ever having to stop the heart or put the patient on a heart-lung machine.”
And that’s the point – to fix the heart with as little disruption as possible.
“Open heart surgery does work very well, and it is a very good option if it’s your only option,” Justino said. “If you can get the very same result without having the chest opened, without a long scar, without using an artificial machine to circulate blood through your brain, and if you can go home the very same day instead of staying in the hospital for several days – even go to school the next day – why would you not want that?”
After three years of development, Justino, Harrington and Chun have a working prototype and are very close to completing their first milestone, which is to prove that it works in the lab setting and meets the criteria the FDA requires of valves. The next phase is animal testing: How does this device perform when it’s placed in a living organism, in contact with organs, tissue and blood? The final step, human testing, may be several years away depending on funding and how well the first two stages go.
“Our long-range goal, after all of this is complete, is to see if we can coat the valve with living tissues and various kinds of cells to make the device more biocompatible with the patient, similar to what Dr. Jacot and his team are doing,” Justino said. “But that’s a long way away. For now, our main goal is to get the best performance we can from this valve and then get it on the market – helping children – as quickly as possible.”
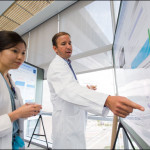
Cutline: Drs. Henri Justino, Daniel Harrington and Kwonsoo Chun examine the prototype valve in a high-cycle tester.