
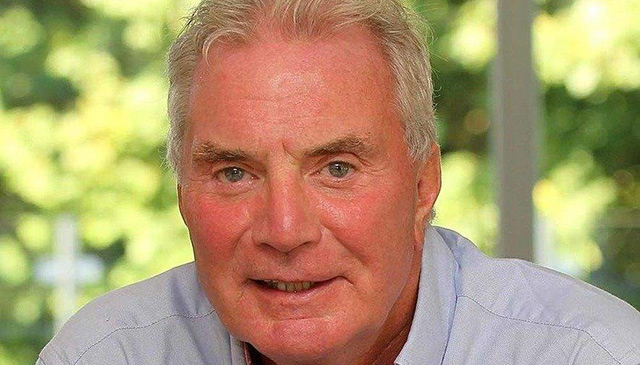
As Dr. Michael Belfort marks his 10-year milestone at Texas Children’s, he reflects on some of his team’s notable accomplishments over the last decade and shares his vision for the future. Read more

As Dr. Michael Belfort marks his 10-year milestone at Texas Children’s, he reflects on some of his team’s notable accomplishments over the last decade and shares his vision for the future. Read more
The story you are about to read is part of an ongoing series about Texas Children’s efforts to care for women and children around the globe. The series highlights Texas Children’s efforts in Malawi, one of the 17 countries we currently serve. Today’s story focuses on the importance of well-trained midwives in Malawi, a county where many babies are born but not enough OB-GYNs are employed.

In Malawi where close to a million babies are born each year, there are only a handful of OB-GYNs to support the midwives and clinical officers who are largely responsible for the care and safe delivery of babies nationwide.
Such is the case at Area 25 Health Center in Lilongwe, the country’s capital, where a unique private-partnership between Texas Children’s, Baylor College of Medicine Children’s Foundation-Malawi and the Ministry of Health of Malawi has made great inroads.
Part of Area 25 Health Center’s success is its midwifery training program led by Rachael MacLeod, a highly skilled midwife from England who has spent many years in Malawi sharing her skills. Hired in March 2019 to oversee the program at Area 25 Health Center, MacLeod is a hands-on mentor who works alongside the midwives she is training. She is also leading an in-depth educational program based on the International Day of the Midwife topic ‘Midwives: Defenders of Womens’ Rights,’ which highlights the vital role that midwives play in protecting the rights of women and girls by ensuring they can exercise their full human rights, particularly their reproductive and sexual health rights in their communities and countries of practice.
“I firmly believe that the way women are treated and cared for throughout their pregnancy plays a huge part in the outcome of their labor,” MacLeod said. “If you care for a women in a centered way, it makes a difference, and that is what we are teaching and doing here at Area 25.”
MacLeod’s students come to her via Malawi’s Ministry of Health’s District Health Office. They spend anywhere from six months to a year at Area 25 Health Center learning in the classroom, the Maternity Waiting Home, on-site OB-GYN Clinic, and Labor and Maternity Ward.
Rose Swai, a midwife and the manager of the Labor Ward at Area 25 Health Center, has worked with MacLeod since she arrived at the Health Center and said the vast amount of knowledge and information she provides both to the existing midwives and the midwives in training is invaluable.
“Rachel is a very experienced midwife,” Swai said. “She’s also a very good teacher, one who truly wants you to understand how to care for your patients in the best possible way.”
In addition to helping train midwives, Swai said MacLeod is helping her standardize the way things are done in the Labor and Delivery Ward, which was recently upgraded to nine beds situated in private rooms, providing women a private place to give birth, and clinical workers more space to deliver the same amount of babies per year born at the Pavilion for Women.
These efforts, and the work of so many others, has caused word about the health center to travel across the region As a result, the number of babies delivered has gone up exponentially over the past few years reaching more 6,000 this year.
The focus on holistic care and the addition of a four-room operating theater is also helping reduce the number of maternal and fetal deaths in the area, Women and children are disproportionately affected by lack of access to health care services, particularly in resource limited settings. Malawian women have some of the worst odds with 675 deaths per 100,000 live births – among the highest maternal mortality ratios in the world. By contrast, the ratio for US women is 14 deaths per 100,000 live births.
To improve these odds, the Global Women’s Health program has invested a lot of time and effort into expanding the quality and quantity of services offered at Area 25 Health Center, significantly alleviating the burden of increasing demand for maternal and neonatal services at Kamuzu Central Hospital (Lilongwe’s referral hospital) and Bwaila Maternity Hospital, the largest maternity unit in the region with 17,500 plus deliveries per year.
Formed in 2012, the Global Women’s Health program is a collaboration between Texas Children’s Hospital, Baylor College of Medicine Children’s Foundation- Malawi and the Ministry of Health of Malawi. This public-private partnership leads the way in the development of transformative programs that benefit thousands of women and babies as well as scores of learners in low resource settings – including midwives.
“I believe in strong partnerships and I believe what Texas Children’s, Baylor and the Malawi government is doing here at Area 25 is working,” MacLeod said. “The majority of the women who come here leave with a healthy baby, a wealth of knowledge on how to care for that baby, and most importantly, a compassionate, caring birthing experience to look back on.”
https://www.texaschildrens.org/blog/working-lockdown
Read more about MacLeod’s experience during the pandemic in her recent blog.
For more information about Area 25 Health Center, click here. To make a donation to Texas Children’s global health efforts, click here.

For the fifth year in a row, the OBGYN Department at The Center-Greenspoint has earned the Patient-Centered Specialty Practice designation from the National Committee for Quality Assurance (NCQA).
The practice was the first in Texas to receive such a designation in 2013 and has continued to become re-designated every year.
“This recognition means that we are who we say we are,” said Dr. Erica Giwa, medical director of the program. “The needs of our patients is our first priority and we deliver programming that supports that. We are so honored.”
Specifically the practice was recognized for setting standards that ensure quality, implementing programs that promote quality, improving vaccination rates and much more.
The award-winning team is a multi-disciplinary one comprised of MDs, pharmacists, behavioral health specialists, care coordinators, nurses and administrative staff.
The Center for Children and Women is part of Texas Children’s Health Plan. The two Center locations are full-service clinics for Health Plan members only, with a few exceptions for members of other government-sponsored programs.
For more information about The Center visit jointhecenter.org
Baylor College of Medicine Obstetrics & Gynecology Grand Rounds will host a talk on Women: The journey is far from over from 8 a.m. to 9 a.m. Wednesday, February 19 in Texas Children’s auditorium, B1 level of Texas Children’s Abercrombie Building.
Dr. James Dornan – chair of Health and Life Sciences at University of Ulster in Ireland, and retired chair of Fetal Medicine at Queen’s University of Belfast in the United Kingdom – will be giving the talk with the aim of increasing clinicians’ knowledge and skills related to the latest scientific advances and translational efforts, as well as the unique ethical challenges, in Obstetrics and Gynecology.
Objectives: Explain that women’s rights are human rights and that human rights are women’s rights.
Illustrate that religions are not to blame, but the men who run them are.
Explain that Native American Indians are correct when they said life is out of balance.
Target audience: OB/GYN Faculty, fellows, residents, and medical students.
Educational methods: Educational methods will include lectures, case presentations, literature review, and panel discussion.
Activity evaluation: Participants will be asked to complete a session evaluation.
Accreditation/Credit Designation: Baylor College of Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
Baylor College of Medicine designates this live activity for a maximum of 1.0 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
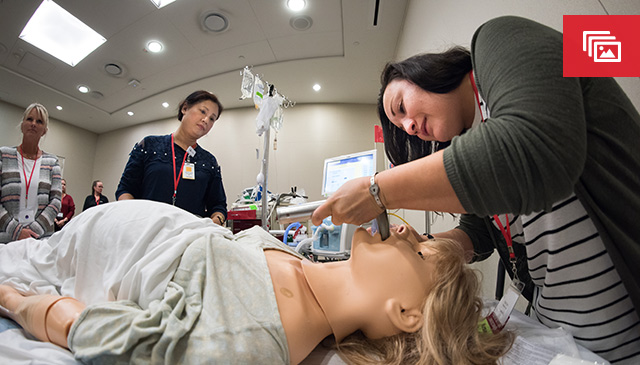
The Pavilion for Women recently held a two-day conference focused on obstetric critical care. With increasing focus on maternal morbidity and mortality the need to expand and elevate the care provided by physicians and nurses is paramount. This unique conference affords the opportunity to participate in skill simulation and expert presentations. Additionally, CMEs and CNEs were awarded upon receiving a successful pass rate of the post-test administered.
Attended by more than 100 people across Texas, and 12 midwives visiting the Pavilion for Women from Hong Kong, the conference covered physiologic changes during pregnancy, specific obstetric medical conditions and appropriate treatment; maternal cardiovascular resuscitation and airway management of critically ill pregnant patients; as well as appropriate steps in fetal assessment, delivery, and neonatal management.
The conference was held October 4 and 5, and was formatted as a series of presentations and skill stations to provide knowledge and guidance for decision-making, and limited practice in some clinical procedures and scenarios. Positively received by attendees, the conference enables the Pavilion for Women as a Level IV Maternal Care Designated facility to determine what educational needs exist across the state and provide additional education to help improve quality outcomes for women.

On January 10, leaders with Texas Children’s Pavilion for Women cut the ribbon on the facility’s new four-bed OB-GYN intensive care unit.
Located in the Labor and Delivery Unit on the ninth floor, the ICU offers a specialized, private space for high-risk expectant and postpartum mothers with conditions such as:
“This beautiful space gives our highly trained clinicians the perfect place to carry out specialized services we’ve offered to our high-risk patients since opening in 2012,” said Lynda Tyer-Viola, vice president of nursing. “Having comprehensive family centered perinatal services in such a setting will help us continue to make a dramatic difference in the lives of expectant mothers with critical complications of pregnancy.”
The Pavilion for Women is home to one of the nation’s few ICUs dedicated solely to obstetric critical care, and the only four-bed maternal ICU in the nation staffed 24/7 by a pulmonary critical care and maternal fetal care team embedded in a hospital’s labor and delivery unit.
The unit’s new space will offer critically ill obstetric patients the latest life-saving equipment and fetal monitoring systems and a dedicated ICU team including 24/7 critical care physicians, maternal-fetal medicine specialists, and an ICU-trained and ACLS (advanced cardiovascular life support)-certified nursing staff.
The ICU team collaborates closely with Baylor College of Medicine subspecialties including cardiology, hematology and nephrology, among others. The unit and team is also one of the most experienced in the nation in the care of post fetal surgery mothers. Uniquely, expectant mothers with a history of cancer or a new gynecologic cancer diagnosis, will also benefit from the expert care and the most advanced treatment therapies available through our renowned colleagues in gynecologic oncology.
“While life threatening illness or medical conditions add to the complexity of any pregnancy, we are fortunate to have a multidisciplinary clinical team and resources that address the needs of both mother and fetus during this very crucial period,” said Dr. David Muigai, medical director of the maternal ICU. “We feel a deep sense of privilege and pride to be able to further contribute to the overall Texas Children’s mission by offering the highest quality and most comprehensive medical services available to expectant mothers and their babies.”
Dr. Manisha Gandhi, chief of maternal-fetal medicine, agreed and said at the ribbon cutting that she was extremely excited about the continued collaboration between disciplines that the new ICU will enable and encourage.
“The need for higher level, specialized care for women has grown exponentially,” Gandhi said. “Having a dedicated space for maternal ICU services will put us in a good place to better serve these patients during this critical time.”
OB-GYN-in-chief Dr. Michael Belfort said the new ICU is an extremely important tool that will help the specially trained clinicians in the unit take care of the sickest of the sick.
“Unfortunately, maternal mortality is increasing in the United States and Texas,” Belfort said. “With this unit, we are better able to care for those who need us the most.”
For more information about the Pavilion’s maternal ICU, the development of which was led by Liz Bolds, assistant clinical director of high-risk nursing, click here.

Dr. Carla Ortique, an OB/GYN with Texas Children’s Pavilion for Women, was recently named physician of the year by the Houston Medical Forum, a component society of the National Medical Association.
The forum was established in 1926 to address the needs of physicians of African descent and their patients. Today, the Houston Medical Forum is the National Medical Association’s largest local affiliate. Its members represent a myriad of specialties and engage in a variety of activities that advance the art and practice of medicine as well as promote education and wellness in the community, eliminate health disparities and sustain physician viability.
“I feel incredibly blessed and honored to be recognized by this organization,” Ortique said.
Ortique earned a B.S. in bacteriology from the University of Wisconsin-Madison in 1982 and her medical degree from the University of Illinois College of Medicine in 1986. Ortique completed an internship and residency in family medicine at the University of Illinois.
A strong interest in providing comprehensive care for women, coupled with the personal experience of having a sister diagnosed with breast cancer, resulted in Ortique undertaking a second residency program. She completed her training in obstetrics and gynecology at St. Paul Ramsey Medical Center in St. Paul, Minn., in 1995.
Ortique has been in the active practice of obstetrics and gynecology in Texas since August 1995. Board-certified in obstetrics and gynecology since 1997, she incorporates her family medicine training as well as training in complementary and alternative therapies to provide comprehensive care to female patients. Her areas of special interest include spirituality and medicine, general obstetrics, minimally invasive surgical procedures including hysteroscopy and laparoscopy, preventative health care and patient safety, guidance for perimenopausal and menopausal patients. Ortique also is interested in health equity and elimination of racial and ethnic health care disparities and elimination of preventable maternal deaths.