The neonatal team at Texas Children’s Pavilion for Women is always prepared for special deliveries – taking care of newborns is what they’re trained to do. But earlier this month, the neonatal intensive care unit (NICU) received a special delivery that wasn’t quite what you’d expect.
The neonatal team at Texas Children’s Pavilion for Women is always prepared for special deliveries – taking care of newborns is what they’re trained to do. But earlier this month, the neonatal intensive care unit (NICU) received a special delivery that wasn’t quite what you’d expect.
Texas Children’s Simulation Center hosted an open house to introduce Tory, a high-fidelity infant mannequin, and the newest addition to the first-ever Neonatal Comprehensive In Situ Simulation Program launched at the Pavilion for Women’s Newborn Center. The simulation equipment and supplies were purchased with a generous $200,000 grant from the M.D. Anderson Foundation, which will also support an in situ simulation program for the Emergency Center and Critical Care, as well as one for the NICU in West Tower once a dedicated space for simulation has been identified.
“We’re grateful to our Newborn Center leadership for dedicating a simulation room at the Pavilion,” said Dr. Jennifer Arnold, medical director of the Simulation Center. “Now, our NICU providers can train in their actual practice environments during regular workdays to enhance individual and team performance – particularly in high-risk situations – and improve patient outcomes and safety.”
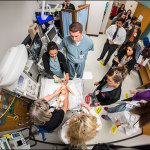
The in situ simulation program focuses on improving crisis resource management skills, one of which is role clarity. During a code, the potential for confusion and chaos can easily set in as responders attempt to care for a patient in a high-risk medical emergency. Clinicians responding to a code may not always be sure of their roles or the roles of their team members when they arrive, and that’s when in situ simulation training becomes crucial to patient safety and care.
“First, we conducted tests to determine the necessary roles in a crisis, whether it’s a resuscitation or a code,” said Dr. Mona Khattab, one of the in situ simulation program directors for the NICU. “By having the necessary personnel at the code, we alleviate staff overcrowding and ensure optimal efficiency and clear communication are achieved while delivering lifesaving treatment to our NICU patients.”
Inside the simulation room, colored labels – red, yellow and green – are affixed to the floor that encircle the bedside. These labels identify the specific roles of each of the code response participants and directs them to their position on the floor during a medical emergency.
- The red team consisting of clinicians and nurses stand in the innermost circle closest to the bedside where they provide direct patient care.
- The yellow team is positioned behind the red team. They support patient care providers by documenting the code, handing over equipment, managing the ventilator and medication and blood prep drawers, and providing mentorship and consultations to the team leader as needed.
- The green team stands in the back of the room near the code cart and provides overall code and room support to ensure everything is running seamlessly.
“When a text message page is sent, the unit reports to the simulation room as if it were an actual page in the unit to respond to a code,” said Kellie Kainer, assistant director of Nursing for the NICU at the Pavilion for Women. “We give them a brief history of the patient and alert them to the code.”
The in situ simulations will occur every Thursday and last 10 minutes followed by 20 minutes of debriefing. The NICU teams alternate every week and are selected based on their current assignment and the flow of the unit on that particular day.
“We’re focusing on one specific patient case so that everyone gets exposure to that case,” said Dr. Leigh Ann Cates, a neonatal nurse practitioner and a program director for the in situ simulation program. “As our program expands, we hope it will become a model for in situ simulations in other units of the hospital.”
In preparation for this training, all clinicians within the Newborn Center complete an online pre-simulation course through Healthstream. The Simulation Center developed a series of powerpoint presentations covering crisis resource management skills, an orientation to simulation, and what to expect during simulation such as a confidential and psychologically safe learning environment.