 Over the course of a two-and-a-half-day meeting in late February, 18 Texas Children’s system leaders came together to strategize streamlining business operations between Texas Children’s Hospital and the Texas Children’s Health Plan. Led by Lou Fragoso, president of the health plan, and Richelle Fleischer, senior vice president of Revenue Cycle at Texas Children’s Hospital, the group worked to challenge business as usual, with an eye toward transforming how the system runs.
Over the course of a two-and-a-half-day meeting in late February, 18 Texas Children’s system leaders came together to strategize streamlining business operations between Texas Children’s Hospital and the Texas Children’s Health Plan. Led by Lou Fragoso, president of the health plan, and Richelle Fleischer, senior vice president of Revenue Cycle at Texas Children’s Hospital, the group worked to challenge business as usual, with an eye toward transforming how the system runs.
This “rapid improvement event,” organized and facilitated by the Texas Children’s Business Process Transformation team, was a key step in the We Are Family initiative, a multi-month undertaking by Texas Children’s system leaders committed to breaking down barriers between the hospital and the health plan in an effort to help the organization work more efficiently as a singular entity. Among the working group’s goals was to plot a roadmap of and deconstruct the revenue cycle process between the hospital and the health plan in order to identify waste and collaborate on solutions that will increase the system’s efficacy.
“We sought to take advantage of our ‘system-ness’ to create a seamless interchange of claim processing, with the potential to save over $30 million in the process,” Fleischer said.
The driving force behind this effort is a desire to leverage the shared organizational identity between Texas Children’s Hospital and Texas Children’s Health Plan in order to reach the common goal of improving patient care.
“During the rapid improvement event, we had a room full of people who wanted to do the right thing for Texas Children’s,” Fragoso said. “When we work together, we can reduce unnecessary or duplicative work, improve the member or patient experience, use data to help deliver better health outcomes, and ultimately make Texas Children’s a leading force in advancing how care is delivered.”
“The biggest accomplishment of the event was the building of relationships between the health plan and the hospital team,” echoed Dr. Heidi Schwarzwald, chief medical officer of Pediatrics at Texas Children’s Health Plan. “Opening new lines of communication, creating efficiencies, and reducing waste will allow for more resources to be available for innovation and improvements in care coordination and delivery throughout our system.”
The We Are Family initiative kicked off in December 2017 with the initial process assessment and event design planning phase taking place between January and February 2018. Further implementation planning followed February’s rapid improvement event, with project kickoffs beginning in April. Implementations and transitions are now underway, with reports of these projects’ measurable results expected in Q4.
Of the 71 ideas suggested at February’s event, the team consolidated and selected 14 high-impact solutions, with 12 projects centered around these solutions currently ongoing. One project has focused on improving antiquated communications technology between the health plan and the hospital. The health plan and the hospital previously relied on fax communications to exchange patient information, a cumbersome and time-consuming process.
Based on the collaborative solutions recommended at the rapid improvement event, the system has transitioned to an entirely digital communications process, thereby reducing administrative burden and allowing employees to focus on timely claims processing and communication with members and providers.
“Ultimately, we’re giving our most important assets, our people, time back in their days,” said Dr. Lia Rodriguez, medical director at Texas Children’s Health Plan. “We’re reallocating resources to focus on what we do best: providing our patients and their families with the best care possible.”
Projected improvements resulting from the We Are Family initiative include:
- 25,000 hours saved
- 85,000 fewer phone calls
- 68 percent fewer handoffs
- 11,000 reduced paper claims
- 12,000 faxes eliminated
- 1,200 reduced appeals
“Just imagine if we take the results from our collaborative effort in February and apply that same concept across the rest of our system,” said Fragoso, who revealed that Texas Children’s Hospital and Texas Children’s Health Plan are already working on a second We Are Family initiative, this time focused on improving outcomes and experience for health plan members by using the hospital’s specialty pharmacy. “As we begin to think differently about how we interact, Texas Children’s will redefine what it means to be a health system in the future. When we unite as one amazing team to improve the lives of the families we serve, Texas Children’s has the ability to completely transform the way care is delivered.”



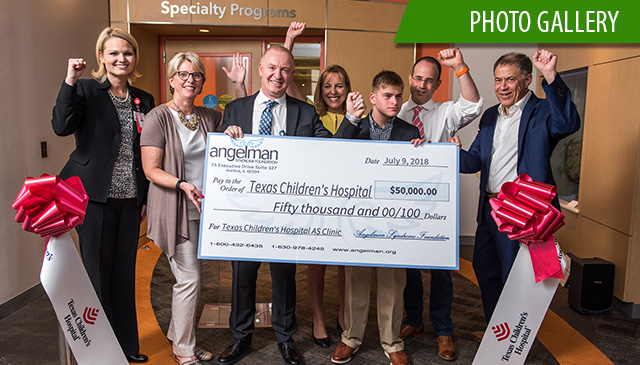 On July 9, Texas Children’s Hospital and the Angelman Syndrome Foundation celebrated the official opening of the Angelman Syndrome Clinic at Texas Children’s, one of only seven Angelman syndrome-specific clinics in the United States – and the first in Texas.
On July 9, Texas Children’s Hospital and the Angelman Syndrome Foundation celebrated the official opening of the Angelman Syndrome Clinic at Texas Children’s, one of only seven Angelman syndrome-specific clinics in the United States – and the first in Texas.















 Texas Children’s Hospital’s Emergency Management and Bone Marrow Transplant teams recently conducted their first large scale functional radiation injury treatment exercise. As a member of the Radiation Injury Treatment Network (RITN), our organization conducts annual exercises as part of our emergency preparedness activities.
Texas Children’s Hospital’s Emergency Management and Bone Marrow Transplant teams recently conducted their first large scale functional radiation injury treatment exercise. As a member of the Radiation Injury Treatment Network (RITN), our organization conducts annual exercises as part of our emergency preparedness activities.



















 “Thanks to online scheduling, it’s super easy to make appointments through MyChart now,” wrote a Texas Children’s family. “The past several times we’ve been here, we have been in and out in less than 45 minutes with the same level of quality and care. It seems like they heard our concerns loud and clear, and it shows that they care.”
“Thanks to online scheduling, it’s super easy to make appointments through MyChart now,” wrote a Texas Children’s family. “The past several times we’ve been here, we have been in and out in less than 45 minutes with the same level of quality and care. It seems like they heard our concerns loud and clear, and it shows that they care.”