When Nurmeen Khokhr called her pediatrician’s office to schedule a time to come in and get the vaccinations she needed before going off to college in the fall, she was pleased to hear she didn’t have to step out of her car.
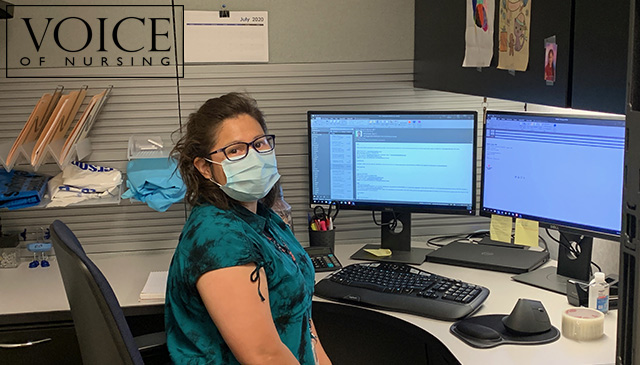
A new program called Car Side Care is being piloted at Texas Children’s Pediatrics Cypresswood in Spring and allows patients nine and older to receive vaccinations from the comfort and safety of their vehicles. All patients have to do is make an appointment, answer a few screening questions, get their temperature taken and roll up their sleeves.
“We are providing the same high-quality care in parking spaces outside our practices as we provide inside our buildings,” said Assistant Vice President Sara Montenegro. “In doing so, we are helping reduce patients’ and staff members’ potential exposure to COVID-19.”
The idea for Car Side Care followed a national drop in the number of patients coming in to get their routine vaccinations. When asked, many patients and/or their family members sited fear of being exposed to the virus as their reason for delaying their shots.
Dr. Stanley Spinner, chief medical officer and vice president of Texas Children’s Pediatrics, said he doesn’t blame people for being cautious, but emphasized the importance of routine childhood vaccines does not lessen during a pandemic. In fact, Spinner said, children should be getting them now more than ever with back to school and flu season right around the corner.
“Vaccines are arguably the most effective public health measure we have next to clean water,” Spinner said. “They are that important, and with the pandemic, they are even more so. I would hate to see a child sick with both COVID-19 and something else like the flu.”
In addition to routine vaccinations, getting kids inoculated against the flu is one of the main drivers behind Car Side Care. Prior to the pandemic, patients needing a flu vaccine often would call their pediatrician’s office, make a nurse’s appointment, and drop by and get their vaccine. That won’t work today with COVID-19 when so many extra precautions are necessary to limit exposure.
“Our offices are very cautious about safety precautions, and with that, needed creative solutions to see hundreds of children for flu vaccine and childhood immunizations quickly, without needing to come in our facilities,” Montenegro said. “Care Side Care is a perfect way to handle this and to hopefully remain on top of the upcoming flu season by vaccinating as many children as possible.”
Car Side Care was launched as a pilot at Texas Children’s Pediatrics Cypresswood and has grown across more than 15 Texas Children’s Pediatrics sites, as we work closely with our landlords to allocate parking spaces to support this program.
Each location will designate four parking spots a couple of times a week to patients wanting to come by and get their vaccines. An appointment will be necessary as well as a COVID-19 screening. Patients and anyone else in the vehicle will be required to wear a mask. Clinicians will wear a mask, goggles and a protective gown. The program has also been expanded from caring for older children to caring fo children of any age over the past two months.
“Texas Children’s Pediatrics has done a very good job at continually finding ways to provide the care our kids need in the safest possible environment,” Spinner said. “Our families seem very happy with the modifications we’ve made thus far and they seem pleased with our commitment to maintain the quality of care we’ve always provided.”
Khokhr said she was very pleased with her Car Side Care experience. It was convenient and gave her the sense of safety she needed to get the shots required by her school.
“I’m glad Texas Children’s Pediatrics is doing this,” she said. “I think it will help ease the nerves of a lot of patients who want to come in and get their vaccines.”