 Angelina Rangel of Nursing Professional Development is the latest Texas Children’s Super Star leader. “A super star is someone who is constantly striving to improve, constantly learning, working to be the best they can be as a person and as a coworker,” Rangel said. “Also this person takes ownership.” Read more of Rangel’s interview and find out how you can nominate a Super Star
Angelina Rangel of Nursing Professional Development is the latest Texas Children’s Super Star leader. “A super star is someone who is constantly striving to improve, constantly learning, working to be the best they can be as a person and as a coworker,” Rangel said. “Also this person takes ownership.” Read more of Rangel’s interview and find out how you can nominate a Super Star
Q&A: Angelina Rangel, October – December 2015 Leader
Your name, title and department. How long have you worked here?
Angie Rangel, MSN, RN, CCRN, LNC – Assistant Director of Nursing Professional Development. I have been at Texas Children’s Hospital for 24 years.
What month are you Super Star for?
October – December 2015
Tell us how you found out you won a super star award.
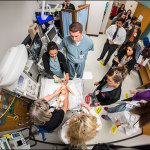
My leader set up a meeting to discuss events for the week. He asked me meet him in the conference room. When I arrived at the conference room, the entire team from Nursing Professional Development was there to surprise me with cake, food and gifts.
What does it mean to be recognized for the hard work you do? How has the organization helped you achieve your personal and professional goals?
I was touched and honored by this recognition. Prior to being employed at Texas Children’s, one of my personal goals was to find an organization where I felt good about going to work. A positive work environment gives any employee motivation throughout the day. I started my career at Texas Children’s as a registered nurse in the NICU-3 in 1991. Honestly I don’t remember a day when I did not feel valued and appreciated by my coworkers and leaders. In turn, I appreciate all of my colleagues as well. With the support of Texas Children’s Hospital’s tuition reimbursement program, I was able to go back to school for MSN/MBA and advance my career from bedside nurse to charge, preceptor, educator, manager and currently as the assistant director of Nursing Professional Development. In every role that I have held, I have felt appreciated and recognized for even the small things that I felt that really didn’t matter. Texas Children’s is a great place to work.
What do you think makes someone at Texas Children’s a super star?
Someone who is constantly striving to improve, constantly learning, working to be the best they can be as a person and as a coworker. Someone who takes ownership, and apologizes if appropriate. Someone who brings high energy, commitment and enthusiasms that causes others around them to respond positively.
What is your motivation for going above and beyond every day at work?
When one feels valued and appreciated, it is a natural motivation to go above and beyond.
What is the best thing about working at Texas Children’s?
As social beings, we naturally seek support from our peers and seek to belong to a group. I found the sense of unity with every team that I have had the privilege of working with at Texas Children’s. A strong team spirit. I appreciate the acceptance and tolerance of differences in perspectives and working styles between team mates. I especially am blessed to be working alongside my current teammates and leaders. There is such cohesiveness among this team.
What does it mean to you that everyone at Texas Children’s is considered a leader? What is your leadership definition?
It means that everyone has a voice. It means leading a life of action. Taking action in your own life, and making the changes that you want to see and focusing on the things you can control. Leadership is a style of persuading. It is about setting an example of inspiration and service. A true leader is a servant, ethical and authentic.
Anything else you want to share?
Many years ago my father told me “if you want to be a leader, you need to be a servant”. Although at that time, I didn’t understand his statement. But later I understood exactly what he meant. The idea of servant leadership isn’t new. Robert K. Greenleaf first coined the term servant-leadership in a 1970 essay.
In his works, Greenleaf discusses the need for a better approach to leadership, one that puts serving others – including employees, customers, and community – as the number one priority. Servant leadership emphasizes increased service to others, a holistic approach to work, promoting a sense of community, and the sharing of power in decision making. In his works, Greenleaf discusses the need for a better approach to leadership, one that puts serving others – including employees, customers, and community – as the number one priority. Servant leadership emphasizes increased service to others, a holistic approach to work, promoting a sense of community, and the sharing of power in decision making.
Some of the characteristics of the servant leader are what I see in the leaders that I work with at Texas Children’s. I have seen the servant leader characteristics in the staff from environmental services to Mr. Mark Wallace. That is why this organization is where it is today. I thank God that I am part of this great organization with leaders who exhibit the philosophy and model of a servant leader. Some of the characteristics of the servant leader are what I see in the leaders that I work with at Texas Children’s. I have seen the servant leader characteristics in the staff from environmental services to Mr. Mark Wallace. That is why this organization is where it is today. I thank God that I am part of this great organization with leaders who exhibit the philosophy and model of a servant leader.
 Pathologists and clinical laboratory scientists at Texas Children’s and Houston Methodist Hospital developed the nation’s first hospital-based rapid test for the Zika virus in a matter of weeks as part of the L.E. and Virginia Simmons Collaborative in Virus Detection and Surveillance.
Pathologists and clinical laboratory scientists at Texas Children’s and Houston Methodist Hospital developed the nation’s first hospital-based rapid test for the Zika virus in a matter of weeks as part of the L.E. and Virginia Simmons Collaborative in Virus Detection and Surveillance.















 Chief of Pediatric and Adolescent Gynecology Dr. Jennifer Dietrich has been voted president-elect of the North American Society for Pediatric and Adolescent Gynecology.
Chief of Pediatric and Adolescent Gynecology Dr. Jennifer Dietrich has been voted president-elect of the North American Society for Pediatric and Adolescent Gynecology.