 Flu season is almost here! While a record breaking 91 percent of our employees received their flu vaccine in 2017, we continue to strive to make the flu vaccination program even more successful. This year we have a lot of exciting new plans to share with you, such as an increased amount of flu vaccination events across the organization and a new online process for employees to submit proof of vaccinations. As a way to encourage our workforce to get vaccinated earlier in the season, all staff who receive their flu vaccine by Friday, November 2, will be entered into a drawing to win one of 25 Nutri Ninja Pro Blenders.
Flu season is almost here! While a record breaking 91 percent of our employees received their flu vaccine in 2017, we continue to strive to make the flu vaccination program even more successful. This year we have a lot of exciting new plans to share with you, such as an increased amount of flu vaccination events across the organization and a new online process for employees to submit proof of vaccinations. As a way to encourage our workforce to get vaccinated earlier in the season, all staff who receive their flu vaccine by Friday, November 2, will be entered into a drawing to win one of 25 Nutri Ninja Pro Blenders.
The Centers for Disease Control and Prevention (CDC) predicts this year’s flu season will begin in October. The CDC recommends a yearly flu vaccination as the first and most important step in protecting against the flu and its potentially serious complications. To learn more about the upcoming flu season, click here. Please remind staff that receiving a flu vaccine protects our patients and their families, reduces flu illnesses, doctor’s visits and missed workdays, and; helps to prevent flu-related hospitalizations.
Below is a more in-depth overview of what to expect for our Flu Program in 2018.
Flu Program Details
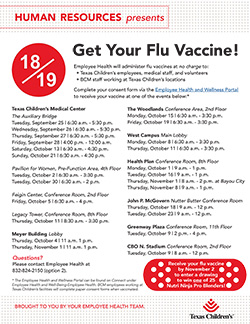
- Employee Health will administer free flu vaccines to Texas Children’s employees, Baylor College of Medicine employees working at Texas Children’s facilities, Morrison, Crothall, or Compass contract employees and volunteers of Texas Children’s Hospital. Employee Health will administer free flu vaccines to Texas Children’s employees, Baylor College of Medicine employees working at Texas Children’s facilities, Morrison, Crothall, or Compass contract employees and volunteers of Texas Children’s Hospital.
- Click on the graphic to the right to view Texas Children’s vaccination event schedule.
- Upon vaccination at Texas Children’s, staff will receive a 2018-2019 flu season sticker to place on their badges. Upon vaccination at Texas Children’s, staff will receive a 2018-2019 flu season sticker to place on their badges.
- Employees who receive their flu vaccine by November 2, 2018, will be entered into a drawing to win one of 25 Nutri Ninja Pro Blenders. Employee Health will email winners at 3 p.m. on Wednesday, November 7.
- In order to protect our patients from exposure to influenza, employees who decline the flu vaccine for approved exemptions should wear a surgical mask when providing direct patient care services for the duration of the influenza season. See In order to protect our patients from exposure to influenza, employees who decline the flu vaccine for approved exemptions should wear a surgical mask when providing direct patient care services for the duration of the influenza season. See Required Influenza Vaccination Policy and Procedure for more details.
Online Consent Form and Proof of Vaccination
- Texas Children’s employees are to complete their Flu Vaccine Consent Form online via the Employee Health & Wellness Portal prior to attending a flu vaccination event.*
- This process greatly reduced the wait times for flu vaccination last year, as well as eliminated the need to scan or fax the Flu Vaccine Consent Forms to Employee Health.
- Click here to view a quick video tutorial on how to access the flu vaccine consent form online.
- For instructions on how to log in to the portal click here or click here to view step-by step instructions.
- New Process: Employees who receive their flu vaccine outside of Texas Children’s can easily submit their attestation and proof of vaccination via this online form. Employee Health will no longer accept proof of vaccination via fax or email.
If you have any questions, please contact Employee Health Services at 832-824-2150, option 2.
* Baylor College of Medicine employees working in Texas Children’s facilities will continue to complete paper consent forms when they receive the flu vaccine.


 As part of National Childhood Cancer Awareness Month, Texas Children’s Bone Marrow Transplant Unit (BMT) was transformed for a few hours last week into a full-fledged parade route – music, costumes and all.
As part of National Childhood Cancer Awareness Month, Texas Children’s Bone Marrow Transplant Unit (BMT) was transformed for a few hours last week into a full-fledged parade route – music, costumes and all.



















 Imagine you’re the parent of a newborn with an arm injury. During your admission you’re told not to move the arm and to protect it all times. Now imagine coming back for your clinic appointment and hearing that it’s time to start moving the arm at home – unsupervised. For parents of children with brachial plexus birth palsy, this moment can be daunting.
Imagine you’re the parent of a newborn with an arm injury. During your admission you’re told not to move the arm and to protect it all times. Now imagine coming back for your clinic appointment and hearing that it’s time to start moving the arm at home – unsupervised. For parents of children with brachial plexus birth palsy, this moment can be daunting. Through dedication, hard work, research and partnership, Texas Children’s Newborn Center has lowered its rate of a serious lung condition in premature infants by more than 13 percent over the past year.
Through dedication, hard work, research and partnership, Texas Children’s Newborn Center has lowered its rate of a serious lung condition in premature infants by more than 13 percent over the past year. September is National Suicide Prevention Month and along with continuing to inform people about warning signs, Texas Children’s has recently elevated our prevention tactics with the use of the Columbia Suicide Screening Rating Scale (C-SSRS).
September is National Suicide Prevention Month and along with continuing to inform people about warning signs, Texas Children’s has recently elevated our prevention tactics with the use of the Columbia Suicide Screening Rating Scale (C-SSRS).







 The National Committee for Quality Assurance (NCQA) recently accredited Texas Children’s Hospital’s Centralized Credentialing Office.
The National Committee for Quality Assurance (NCQA) recently accredited Texas Children’s Hospital’s Centralized Credentialing Office.