 Hearing the words, “you’re pregnant” can be an exciting, life-changing moment. But for many couples struggling with infertility, the journey to parenthood is frustrating, stressful, and can at times feel hopeless.
Hearing the words, “you’re pregnant” can be an exciting, life-changing moment. But for many couples struggling with infertility, the journey to parenthood is frustrating, stressful, and can at times feel hopeless.
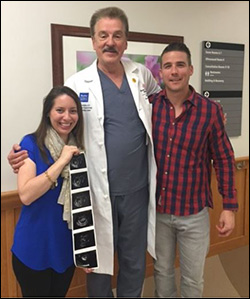
For almost two years, Brooke Schmitt and her husband, Daniel, struggled to start a family, but infertility issues got in the way of achieving their dream of parenthood.
“My OB/GYN ran several tests, and it turned out that my numbers were really low,” Brooke said. “Since my ovaries were not releasing eggs, my doctor recommended that I consult with a fertility specialist.”
After consultations with other providers, Schmitt chose the Family Fertility Center at Texas Children’s Pavilion for Women, a regional and national leader in providing advanced fertility services to families who have had difficulty conceiving.
Since opening in July 2014, the center’s reputation was strengthened even more in 2016 when its success rates for in-vitro fertilization (IVF) reached a milestone – 47 percent of embryo transfer patients at the Center achieved clinical pregnancy.
Dr. William Gibbons, chief of Reproductive Medicine at the Pavilion for Women and founding director of the Family Fertility Center, credits the Center’s success to numerous factors – state-of-the-art technology, research and support of Texas Children’s Hospital.
“Texas Children’s allowed me to have resources that many IVF programs don’t have,” Gibbons said. “They enabled us to build the absolute best lab that we could have, and we have almost as much research lab space as clinical lab space.”
The Family Fertility Center is the first in Houston and among the early adopters in the U.S. to offer the EmbryoScope, an embryo monitoring system that provides continuous moving time-lapse images of embryos as they grow. This technology allows fertility specialists to identify the healthiest embryo to transfer to the patient to improve IVF success.
Realizing the uncertainties that often accompany fertility treatments, the Schmitts relied on the Center’s expertise and state-of-the-art capabilities to help facilitate their dream of becoming parents. After consulting with their reproductive endocrinologist Dr. Paul Zarutskie, Brooke and her husband elected to pursue IVF.
“I was really lucky – my numbers were great,” Brooke said. “They retrieved about 41 eggs, and 39 of them fertilized successfully.”
At the end of day five, 12 of Brooke’s embryos were still living. All of them underwent genetic testing, and five of them were healthy. She and her husband, Daniel, implanted an embryo. The other four healthy embryos were cryogenically preserved for future implantation.
Brooke was implanted with an embryo on February 5, 2016. After undergoing blood work to confirm the couple was pregnant, the test came back positive.
Their daughter, Sophia, was born October 19, 2016.
“It’s a surreal feeling to know that you’re a parent and you’ve made this baby,” Brooke said. “We know we couldn’t have made her without the help of Dr. Zarutskie and the fertility team. Between the talent and the state-of-the-art technology there, it was a perfect combination that produced a perfect outcome.”
To read more about the Schmitts’ story in Texas Children’s Annual Report, click here. To learn more about Texas Children’s Family Fertility Center, click here.




