December 5, 2017
 On November 21, Texas Children’s earned The Joint Commission’s Gold Seal of Approval for Palliative Care Certification, making Texas Children’s Palliative Care Program the first of its kind in Houston and one of only 90 across the United States to receive such a distinction.
On November 21, Texas Children’s earned The Joint Commission’s Gold Seal of Approval for Palliative Care Certification, making Texas Children’s Palliative Care Program the first of its kind in Houston and one of only 90 across the United States to receive such a distinction.
The certification demonstrates Texas Children’s focus on achieving optimum care for patients with serious illnesses and is a symbol of quality that reflects an organization’s commitment to providing safe and effective patient care.
The Palliative Care team recently underwent a rigorous onsite review during which Joint Commission experts evaluated compliance with national palliative care standards built on the National Consensus Project’s Clinical Practice Guidelines for Quality Palliative Care and the National Quality Forum’s National Framework and Preferred Practices for Palliative and Hospice Quality Care.
“Texas Children’s has demonstrated its commitment to serve patients diagnosed with a critical and debilitating illness in a safe, high quality and patient-focused environment,” said Patrick Phelan, executive director, Hospital Business Development, The Joint Commission. “We recognize and commend Texas Children’s for its efforts to provide palliative care services while emphasizing patients’ physical, emotional and spiritual needs as they make end-of-life decisions.”
Established in 2011, The Joint Commission’s Palliative Care Certification is awarded for a two-year period and recognizes organizations that demonstrate exceptional patient and family-centered care in order to optimize the quality of life for patients with serious illnesses.
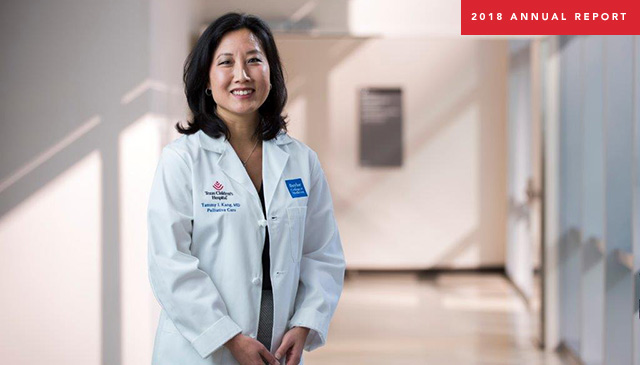
“Texas Children’s is pleased to receive certification from The Joint Commission, the premier health care quality improvement and accrediting body in the nation,” said Dr. Tammy Kang, section chief of Palliative Care at Texas Children’s. “The certification recognizes hospital inpatient programs and helps to further promote and advance the field of palliative care, ultimately improving the care for persons living with serious illnesses.”
Helping parents verbalize their challenges and focus on what they want to accomplish with their seriously ill child are among the goals of the system-wide Palliative Care program at Texas Children’s Hospital.
“What we have tried to promote is the understanding that palliative care is about maximizing quality of life, and improving care and support for children and families with serious illness, regardless of prognosis,” said Kang, who holds a clinical epidemiology degree and was recruited from the prestigious Children’s Hospital of Philadelphia, where she started a palliative care team and managed it for the past 15 years. She launched the clinical service at Texas Children’s in October 2016.
Clearing up misunderstanding
“Many people have the misunderstanding that palliative care is hospice care or end-of-life care,” Kang said. “We certainly partner with hospice agencies in the community to provide those kinds of services, if that’s what the patient is facing and that’s the family’s choice. But the vast majority of children served by pediatric palliative care providers are not in hospice care and are not terminal. Instead, these are children with complex, serious illness who require additional support and services for managing distressing symptoms. It’s for helping families understand the medical processes and interventions, for providing psychosocial, spiritual and emotional support for patients, their families and their siblings. And it’s just helping families navigate this very complicated health care system.”
To provide that support takes an interdisciplinary team of physicians, nurses, social workers, child life specialists, chaplains and other support specialists.
“Many of the kids have issues with multiple organ systems, where they have 20 or 30 medical problems” said Dr. Daniel Mahoney, a palliative care physician. Sometimes the course of treatment, such as chemotherapy or bone marrow transplants, may cause problems in the heart or kidneys. A problem in the genetic code can affect every organ system in the body – the brain, heart, lungs, kidneys and liver.
“Often kids have multiple specialists who try to coordinate care,” Mahoney said.
Long-term attitude
Although the formal, system-wide Palliative Care program is somewhat new at Texas Children’s, individual palliative care programs existed in several service lines. And, of course, working as a team to provide the best care for very sick children is not a new concept at Texas Children’s.
A landmark report published in 2000 by the Institute of Medicine, When Children Die: Improving Palliative and End of Life Care for Children and Their Families, stimulated work across the country to improve palliative care programs for children.
In the years since then, Texas Children’s has:
- Taught twice a year the End-of-Life Nursing Curriculum, developed from a national Robert Wood Johnson Foundation project;
- Started a perinatal palliative care service for pregnant women facing difficult fetal diagnoses;
- Supported clinicians to attend the Palliative Care and Practice Educational course at Harvard and a retreat presented by the Initiative for Pediatric Palliative Care;
- Started a palliative care service for Texas Children’s Cancer and Hematology Center patients.
Under the leadership of Physician-In-Chief Dr. Mark W. Kline, and with the efforts of Dr. Susan Blaney, deputy director of the Texas Children’s Cancer and Hematology Centers, and representatives with Ethics and Palliative Care at Texas Children’s, the organizational umbrella opened in 2016 with support from Texas Children’s Hospital and Baylor Department of Pediatrics.
Texas Children’s Information Services team also was instrumental, partnering with Epic Production Support to create the necessary tools to improve the care of their patients. This collaboration included the development of a customized navigator, note templates, and letters. These improvements also provided the “Pink Sheet” in an electronic format. The pink sheet, which was previously only available in a paper format, ensures that this patient population is cared for in accordance to county and state regulations. As an added benefit, the new electronic form will streamline workflow by making it easier to identify required documentation. Automation of documentation lets our Palliative Care Team have more time to provide more family centered care.
“One of the things that already existed here is this commitment from the leadership on down to the clinical providers to really provide the best possible care for every patient, for every family, regardless of where they came from, what their diagnosis was, or their prognosis,” Kang said. “What also exists here is this great collaborative energy between the medical teams, the department, the hospital and the hospital administration that’s needed for our integrated way of caring for children.”
The Palliative Care team sees patients across the hospital and its many clinics. In its first year of clinical operation, the team provided more than 435 consults and 1,800 follow-up visits.
“We’ve heard from families that they really appreciate this consultant team helping them identify the goals of care,” said Joy Hesselgrave, a longtime nursing staff member in Hematology-Oncology, who is now assistant clinical director of Palliative Care. “The team listens to what the family thinks they want for their child, listens to the clinical medical team who manages the medical care and who says what’s possible, and then communicates that to the family in a way that helps with their decision-making process.
“I think a lot of families have ideas about what they think, but they haven’t articulated them. They haven’t made any plans or contingencies. Just offering them a space in which to communicate and to clarify is very helpful. It’s not high tech, but high touch is really important.”
Available 24 hours a day
It may not be clear in the first visit how the team can be helpful, but it becomes clear as they get to know the family and build a long-term relationship. The team provides a cell phone number to parents, staff and referring physicians for a phone that is answered 24 hours a day, seven days a week by a physician from the team.
One of the team’s goals is a home visit program, in which psychosocial providers can go to the homes to check on patients, as well as provide support for caregivers and siblings.
“We know that siblings of children with serious illness are at risk for increased health issues, increased learning issues, and increased behavioral and psychological issues,” Kang said. “These children are often going through a lot of difficulties because their parents are at the hospital, and there is a lot of emotional and financial stress in the household. Being able to provide some support for these children in the home is a future goal.”
While physician visits are billed as medical visits, families are not billed for any of the other services.
“We really rely upon philanthropy to allow us to think about how to grow and to provide the best care and the best support both in the hospital and in the community,” Kang said. “I perceive our outcomes as being successful if we are doing our very best for every patient and every family that walks through the door.”
Significant support for staff
In addition to caring for patients and families, the team helps support staff.
“We didn’t really anticipate support for staff as being so significant,” Hesselgrave said. “To take care of and be the witness and the caregiver for children who are very sick or dying is very emotionally, physically and mentally exhausting. It’s very helpful to have members of our team there walking the journey with them.”
Besides emotionally supporting the staff, the team provides education about palliative care to staff at Main Campus, The Woodlands and West Campus. The program received Accreditation Council for Graduate Medical Education accreditation for a fellowship program in pediatric hospice and palliative medicine in 2016 and is training its first fellow. Beginning next year, the team will be able to train two fellows per year. They anticipate broadening their reach within the hospital and to community physicians and home care providers, educating them on the benefits of palliative care.
“We are committed to developing a research and outcomes platform as well,” Kang said. “We are well poised at Texas Children’s, because it is the largest academic pediatric program in the country, to help move the palliative care field forward through actively engaging in educational and research opportunities. A number of researchers across this institution right now have research interests relevant to palliative care, where I think important questions could be answered here relatively quickly.”
Putting its large, diverse patient population to good use for research, Texas Children’s is a member of the Pediatric Palliative Care Research Network, a research group of children’s hospitals in the U.S. and Canada.
In the complex world of medicine, the Palliative Care team leads families and staff through the thicket today and uses research to clear the way for tomorrow.





















































 On November 21, Texas Children’s earned The Joint Commission’s Gold Seal of Approval for Palliative Care Certification, making Texas Children’s Palliative Care Program the first of its kind in Houston and one of only 90 across the United States to receive such a distinction.
On November 21, Texas Children’s earned The Joint Commission’s Gold Seal of Approval for Palliative Care Certification, making Texas Children’s Palliative Care Program the first of its kind in Houston and one of only 90 across the United States to receive such a distinction.