Texas Children’s Hospital and Baylor College of Medicine launch a new clinical genomic sequencing program to help patients with undiagnosable conditions. Read more
Texas Children’s Hospital and Baylor College of Medicine launch a new clinical genomic sequencing program to help patients with undiagnosable conditions. Read more

Every day we make the impossible possible by doing things differently. Click here to see it again.

Pioneering neurologist and Texas Children’s Research-in-Chief Dr. Huda Zoghbi has been awarded the prestigious 2022 Kavli Prize for neuroscience, making history as the first Kavli Prize recipient for both Texas Children’s and the Baylor College of Medicine.
The Kavli Prize is a partnership among the Norwegian Academy of Science and Letters, the Norwegian Ministry of Education and Research and the Kavli Foundation to recognize scientists in astrophysics, nanoscience and neuroscience for breakthroughs that transform our understanding of the big, the small and the complex.
Zoghbi is one of just 11 scientists from around the world to be named a Kavli Prize Laureate this year, in recognition of two groundbreaking discoveries.
The first discovery came with long-time collaborator and University of Minnesota professor Dr. Harry T. Orr, who also received the Kavli Prize. Together, Zoghbi and Orr independently discovered the gene known as ATAXIN1, which is responsible for spinocerebellar ataxia 1 (SCA1). SCA1 is a progressive and often deadly disease in which neurons in the cerebellum and brain stem degenerate, causing loss of balance and coordination as well as swallowing difficulties.
Zoghbi’s second discovery was of the MECP2 gene responsible for Rett syndrome, a developmental disorder that strikes children, mostly girls, causing regression and disability.
“I am deeply honored by this recognition and credit my mentors, trainees, collaborators, and the incredible research environment at Baylor and Texas Children’s Hospital in helping me advance the work on SCA1 and Rett syndrome,” said Zoghbi, who is also the founding director of Texas Children’s Jan and Dan Duncan Neurological Research Institute, a Distinguished Service Professor at Baylor and a Howard Hughes Medical Institute investigator.
“To be acknowledged alongside Harry Orr, Jean-Louis Mandel and Chris Walsh is especially meaningful as it is beautiful recognition of the power of genetics for understanding disease,” she said.
Zoghbi joined Texas Children’s and Baylor in 1983 as a resident in child neurology. After encountering two patients with Rett syndrome and identifying other children with similar symptoms, she was inspired to go into research to uncover what caused the disorder.
While treating Rett syndrome, Zoghbi took note of spinocerebellar ataxia and her research with impacted families led her to Orr – who was also working with families affected by spinocerebellar ataxia. The pair shared techniques from their respective work and discovered the disease-causing gene ATAXIN1 in April 1993.
In 1999, Zoghbi and her research team were able to identify mutations in methyl-CpG-binding protein 2 gene, known as MECP2, as the root cause for Rett syndrome. The discovery of the Rett syndrome gene provided a straightforward diagnostic genetic test, allowing early and accurate diagnosis of the syndrome.
“From the moment Dr. Zoghbi arrived at Texas Children’s Hospital, we knew immediately that she was essential to unlocking the mystery of these devastating diseases,” said President and CEO Mark A. Wallace. “Dr. Zoghbi continues to amaze us with her commitment to not only understanding what causes neurological diseases but also her dedication to lead the discovery and development of new treatments that will undeniably transform the landscape of neurological research and, ultimately, change lives for generations to come.”
For more on Zoghbi, her work and the 2022 Kavli Prize honor, click here.

Texas Children’s Neurosciences Program is all about improving patient outcomes. Every day, our team of neurologists, neurosurgeons, geneticists, physician-scientists and researchers are working together tirelessly to pioneer innovative therapies to improve the lives of children with neurological disorders.
On February 21, neuroscience leadership at Texas Children’s together with faculty and staff convened for the inaugural Neurosciences Retreat at the Jan and Dan Duncan Neurological Research Institute (NRI). This informative and engaging event provided our multidisciplinary team of neurologists, neurosurgeons, clinicians, researchers, behavioral health experts, and more the opportunity to reflect on past successes, discuss areas of possible improvement, identify transformative goals and actively plan for the future.
After welcome remarks from Executive Vice President Dan DiPrisco, the retreat began with a moderated panel discussion with two patient families who shared their inspiring stories that brought them to Texas Children’s Hospital. One of the guests was Debbie Sukin, the daughter of the late Dr. Ralph D. Feigin.
Sukin’s two sons, 18-year-old Jacob and 15-year-old Eli, were born with neurological challenges. Jacob was diagnosed with Angelman’s syndrome and Eli was diagnosed with a very rare neurological disorder caused by a CASK gene mutation diagnosed through genome DNA sequencing at Texas Children’s Hospital and Baylor College of Medicine.
“Texas Children’s holds a very special place in my family’s heart,” Sukin said. “We always knew about the hospital’s focus on clinical care and research, and didn’t quite know at the time that it would be so beneficial and important to our family. We are very much involved, on both the basic science and clinical sides, and the multidisciplinary components that are necessary to care for a child with neurological issues.”
The Sukin family’s journey, like so many other patient family stories shared at the retreat, highlight our clinical and research partners’ collaborative efforts in advancing neuroscience research, ultimately leading to the development of novel treatments and discovery of cures for neurological disorders.
“We’re always striving to do things better, and I think this retreat is one step towards getting us there,” said Texas Children’s Chief of Neurosurgery Dr. Howard Weiner. “Everyone here is ready to embrace a new idea if it’s going to advance the field forward. The key to our success is the ability for everyone – in Neurosurgery and our amazing colleagues in Neurology and the NRI – to work together for our patients.”
Weiner, along with Dr. Gary Clark, chief of Neurology and Developmental Neuroscience, and Dr. Huda Zoghbi, director of the NRI, participated in a panel discussion that highlighted the organization’s bench-to-bedside achievements in neuroscience research and neurological care over the last 20 years, and outlined collaborative opportunities to accelerate innovation and research to improve patient outcomes.
“We’re entering the renaissance of neuroscience in pediatrics,” Clark said. “Neurology and neurosurgery are not the same programs they were five or 10 years ago. Neurological diseases that we thought for years were not treatable, have become approachable with new DNA therapies, enzyme replacement therapy to treat lysosomal disorders, and minimally-invasive surgical approaches like laser ablation, that was pioneered at Texas Children’s, and has yielded successful outcomes for treating epileptic seizures.”
The panel also discussed strategies to ensure a seamless flow from bench to bedside, that will help researchers accelerate the discovery behind the causes of neurological diseases so that effective therapeutic interventions can be developed to improve the quality of life and outcomes for patients.
“At the NRI, our teams have identified the causes of about 66 different neurological disorders, some degenerative, others developmental or psychiatric, and have identified the path for therapeutics,” Zoghbi said. “Together, with our collaborators and trainees, we are charting new paths towards viable therapies that will have an immeasurable impact on families suffering from unexplainable neurological diseases.”
After the panel discussions, attendees split up into pre-selected breakout groups. The teams chose their groups based on the topic, and were tasked with helping to establish neuroscience goals and collectively chart the path for treatments, discoveries and cures to be realized over the next five years
The breakout groups facilitated lively discussion and engagement around these topics:
“One of our goals coming into this retreat was to simply facilitate discussions,” said Senior Vice President Matthew Girotto. “We have world renowned clinical and research teams that, too often, do not connect with each other. By simply bringing everyone together, we were able to uncover several opportunities that could not only help accelerate discovery to improve patient care but also increase our collaboration with Texas Children’s Pediatrics in addressing many of the common neurological needs of children.”

During the final week of October, Texas Children’s Hospital hosted visitors from around the world for a very special Rett Syndrome Symposium and Workshop.
The two-day event was momentous for many reasons. It was the inaugural meeting held in the stunning new Auditorium and Conference Center at the Jan and Dan Duncan Neurological Research Institute (Duncan NRI) at Texas Children’s Hospital. It fortuitously coincided with Rett Syndrome Awareness Month. And the symposium also marked the 20th anniversary of the discovery of the underlying cause of Rett syndrome. In 2000, NRI director Dr. Huda Zoghbi’s research team made the pioneering discovery that loss-of-function mutations in methyl-CpG binding protein, MECP2, were the underlying cause of Rett syndrome.
Rett syndrome is a rare neurological disorder that primarily affects young girls between 6 months and 2 years of age. The children appear to hit normal developmental milestones until, inexplicably, their motor, cognitive and social skills start to rapidly deteriorate. Most patients develop autistic features, breathing difficulties, dementia, growth abnormalities, epilepsy and scoliosis.
The symposium opened with a warm welcome from co-organizers Dr. Adrian Bird – Buchanan Professor of Genetics and Welcome Trust Center for Cell biology at the University of Edinburgh, UK – and Zoghbi, who is also a professor at Baylor College of Medicine and Howard Hughes Medical Institute investigator.
“The purpose of this event was to bring together researchers who work on Rett syndrome and leaders from related areas of neuroscience working in academia, industry and government, to think deeply and spark new ideas,” said Zoghbi. “The hope is that out of the work and discussions that happened here, in five years, when we’re marking the 25th anniversary of the gene discovery of Rett syndrome, we’ll also be celebrating new treatments for people with Rett syndrome.”
The international symposium was sponsored by Rettsyndrome.org (formerly the International Rett Syndrome Foundation) and the Rett Syndrome Research Trust. The multidisciplinary group of attendees included scientists, physicians, members of the lay public, and representatives from the National Institutes of Health, the pharmaceutical industry, and several foundations, all brought together to look at Rett syndrome with a fresh, new perspective.
On the first day of the symposium, presentation topics ranged from clinical observations of MECP2 disorders like Rett and MECP2 duplication syndrome to pathogenesis (progression or development) of Rett syndrome, to discussions on neuronal circuit alterations and therapeutics. Texas Children’s pediatric neurologist Dr. Bernhard Suter spoke about MECP2 duplication syndrome, which typically affects male patients and causes symptoms such as hypotonia, motor delays, intellectual disabilities, gastrointestinal issues and epilepsy.
Following a day of stellar research presentations, the investigators split into three working groups that focused on Molecular Pathogenesis, Therapeutic Approaches and Young Investigators. The groups discussed the information presented over the course of the day and their vision for the future of Rett syndrome research. This included the systemic and technical challenges that currently exist, and the group brainstormed ways to overcome those. The next morning, key points from these discussions were shared with the audience.
Learn more about Texas Children’s research efforts at the Jan and Dan Duncan Neurological Research Institute and world-class clinical expertise provided at the Rett Center.

The Jan and Dan Duncan Neurological Research Institute (NRI) at Texas Children’s Hospital recently hosted the first-ever family conference for EBF3-HADD (Hypotonia, ataxia and delayed development) syndrome (HADDS). Medical residents, genetics counseling students and research scientists joined more than 20 families from across North America that attended in person and 13 families that participated via live-streaming services from countries around the world – including Ireland and Australia – making it a truly international event.
The conference was organized by the EBF3-HADDS Foundation, a nonprofit organization created in 2018 by families to promote awareness, research and support for this genetic syndrome. The foundation was co-founded by Ashley LeMaire and her husband, Mark. After one of their children was diagnosed with HADDS in 2016, the LeMaires started a Facebook group for HADDS families. In just two years, that group has grown into an international community and was the impetus behind the foundation’s creation.
“Our HADDS community is a motivated and talented group of families dedicated to supporting research, education and advocacy efforts for HADDS patients, and we support each other on this journey,” said LeMaire, who is a clinical neuropsychologist at the Menninger Clinic, assistant professor of Psychiatry & Behavioral Sciences at Baylor College of Medicine, and also board member of the EBF3-HADDS Foundation. “There is still much to learn about HADDS, but when you have such a dedicated team of physicians and researchers collaborating with families to learn about the condition and provide needed support, it fosters so much hope for our families.”
During the conference, guests attended presentations on a variety of HADDS-related topics given by NRI researchers Drs. Hsiao-Tuan Chao and Michael Wangler; pediatric urologist Dr. Irina Stanasel, a former Texas Children’s fellow; Texas Children’s genetic counselor Pilar Magoulas; and Geraldine Bliss, research director of the Phelan-McDermid Foundation. Additionally, Chao and Wangler offered clinical evaluations for patients, and attendees were also able to tour research labs and facilities at the NRI, where one of the first genetic discoveries for HADDS was made in 2016, and the first lab (Chao’s) devoted to understanding the biology of this disorder.
If you’ve never heard of HADDS, there’s a good reason. The rare genetic disorder, caused by a mutation in the EBF3 gene, was only discovered in 2016 by Chao and Wangler when they were training in NRI investigator Dr. Hugo Bellen’s lab, in collaboration with colleagues at the Undiagnosed Diseases Network (UDN) and New York University Langone Health.
The UDN had been stumped by a case in which a child exhibited symptoms including impaired speech and cognition, low muscle tone, balance and gait issues, reduced ability to feel physical pain, and an inability to show facial emotional expressions. Though earlier DNA sequencing had yielded a few candidate genes, there wasn’t a significant patient cohort or research to help determine which gene was responsible for the symptoms.
Researchers selected EBF3 as the most likely candidate gene. Chao then used fruit flies to mimic mutations to better understand EBF3’s role, and within a few months three patients were found who presented with similar symptoms and similar mutations in the EBF3 gene.
As result of those efforts, more than 200 patients with HADDS have been identified to date.
“The gene discovery of EBF3 illustrates the ‘Power of One’ in medicine and biomedical research, how a single patient with an undiagnosed disorder – a ‘medical mystery’ – can lead to the discovery of a gene responsible for a previously unknown disorder,” Chao said. “This becomes the starting point to develop the diagnostic tests and therapies that can transform the lives of many patients and their families.”
Since 2017 Chao and Wangler have offered monthly clinical evaluations for HADDS patients at Texas Children’s and have now seen the largest number of such patients at any single institution worldwide. They are also enrolling patients in a study to better understand the condition and to help translate research into potential clinical interventions in the future.
The conference was a testament to the power of teamwork and collaboration in research, and also shows how dedicated parents and volunteers from across the globe can work together to build a community of support.
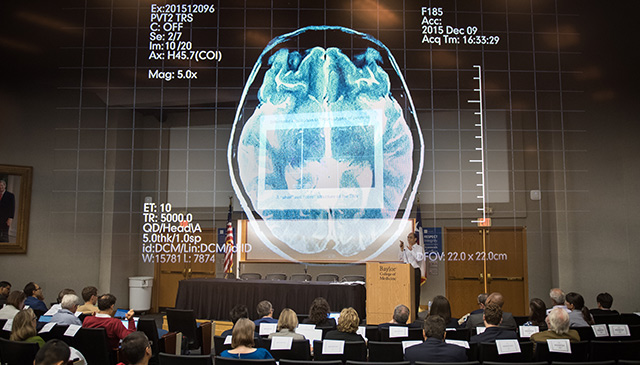
Some of the brightest minds in neuroscience recently converged on the Jan and Dan Duncan Neurological Research Institute (NRI) at Texas Children’s Hospital for its fourth biennial symposium and workshop, in partnership with Baylor College of Medicine.
The special two-day event brought together nearly 300 physicians, scientists, patients, patient advocacy groups, pharmaceutical industry experts and leaders from the National Institutes of Health (NIH), the National Institute of Neurological Disorders and Stroke, and the National Institute for Mental Health, to address key issues in the field of neuropsychiatry, an intersectional branch of medicine that deals with mental illnesses caused by organic disorders of the nervous system.
Neuropsychiatric disorders are a leading cause of disability and take a tremendous toll on society. In the United States alone, one out of five adults lives with mental illness. The spectrum of mental illnesses is vast, ranging from the extremely rare to more well-known conditions such as depression, anxiety, schizophrenia, ADHD, addiction and sleep disorders. Symptoms and their severity can vary widely from patient to patient, which makes them difficult to physiologically measure. For these reasons, neuropsychiatric disorders are some of the least understood – and some of the most difficult to treat.
“These disorders are a major health issue all over the world, however, therapeutic interventions remain limited,” said NRI/Baylor investigator and child neurologist Dr. Hsiao-Tuan Chao. “There is a growing need to understand the organic factors behind mental illness to facilitate a better understanding of the brain, as well as to develop more effective treatment strategies.”
The symposium opened with a welcome address from Dr. Huda Zoghbi, director of the NRI, and this year’s co-organizer, Dr. Steven Hyman, director of the Stanley Center for Psychiatric Research at the Broad Institute of MIT and Harvard. The pair stressed the importance of identifying new research paths in order to develop targeted therapies that could not only help treat neuropsychiatric symptoms, but could also help mitigate or eliminate side effects and toxicities that far too many patients experience.
Over the course of the first day, presentations from leading experts addressed hot topics in neuropsychiatry. These included a discussion on how genetic mutations contribute to neuropsychiatric disorders; the involvement of neuronal networks in neuropsychiatric phenotypes; the impact of immune cells on these disorders; and a look into how adaptive deep brain stimulation could potentially help specific conditions. Each session gave way to a 20-minute moderated panel discussion on the topic at hand. This feature of the symposium is unique in that it leads to immediate discussion and active participation among the many different types of stakeholders present.
Following a day of stellar research presentations, the investigators split into three working groups that focused on Molecular Bases of Disease and Human studies, Circuits and Neuromodulation, and Young Investigators. The groups discussed not only everything they had heard over the course of the day, but also their vision for the next 20 years in neuropsychiatry, including the obstacles that currently exist and what is needed to overcome them.
The next morning, key points that had emerged from these discussions were shared with the audience. The working groups identified increased access to resources and funding as a major need. But unanimously, all of the young investigators noted the critical importance of building interdisciplinary, multi-institutional collaborations, with a focus on team science and data sharing.
“Building bridges between various disciplines aids in the identification of important areas of neuropsychiatry that require further investigation and therapeutic development,” said Chao. “Neuropsychiatry itself is an interdisciplinary field, and unraveling the causes for these conditions will require continued interdisciplinary collaborations to accelerate the pace of discovery.”
The proceedings will be published as a white paper in Science Translational Medicine, a leading weekly online journal and one of the event sponsors.