 Thanks to the more than 10 years of dedication and hard work of neonatologists and neonatal nutrition experts at Texas Children’s, Boston Children’s and the University of California at Los Angeles (UCLA) hospitals, premature babies with liver disease now have better access to a potentially lifesaving drug.
Thanks to the more than 10 years of dedication and hard work of neonatologists and neonatal nutrition experts at Texas Children’s, Boston Children’s and the University of California at Los Angeles (UCLA) hospitals, premature babies with liver disease now have better access to a potentially lifesaving drug.
On July 27, the FDA approved Omegaven®, an omega-3 fatty-acid-rich lipid solution made from fish oil for use in babies suffering from Parenteral Nutrition Associated Cholestasis (PNAC). For over a decade, Texas Children’s and Boston Children’s have been giving Omegaven® to NICU babies with this disease under compassionate use protocols.
Nearly 20 percent of babies in the NICU develop intestinal failure and are dependent on artificial nutrition (total parenteral nutrition or TPN). Of these infants 25 percent to 50 percent of them develop PNAC, a dreaded complication resulting in long term damage to the liver. Prior to the use of Omegaven®, nearly 50 percent of these babies with PNAC developed liver failure and died, or needed a liver transplant. However, since the use of Omegaven®, 85 percent of infants with PNAC have survived long term, rarely needing a liver transplant.
Being first-hand witnesses to this remarkably improved outcome, neonatologists at Texas Children’s long advocated for the approval of Omegaven. Extensive patient data demonstrating the beneficial effects of Omegaven® on the babies with PNAC from Texas Children’s, Boston Children’s and UCLA formed a crucial part of the new drug approval application submitted to the FDA. Now that Omegaven® is approved by the FDA for use in babies with PNAC, hospitals across the country will have access to it, saving many lives.
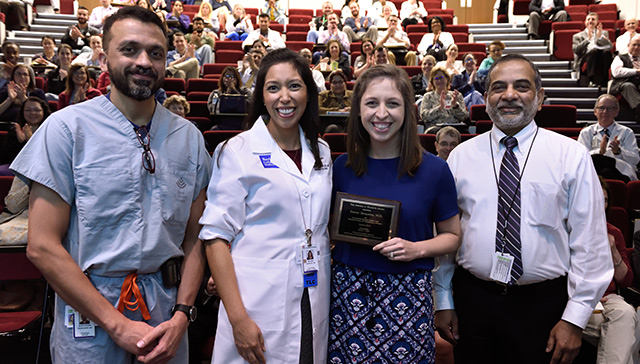
“This is a game changer,” said neonatologist Dr. Muralidhar Premkumar. “I am very confident that Omegaven’s approval by the FDA will tremendously improve the outcomes of infants with intestinal failure.”
Program Director of Neonatal Nutrition Dr. Amy Hair agreed and said the approval is “huge, and will most definitely save babies’ lives.”
Over the past decade, liver transplants have decreased nearly 25 percent nationwide in babies with PNAC, mainly as a result of improved multi-disciplinary care of infants with intestinal failure and the use of safer lipid solutions such as Omegaven®. Texas Children’s Newborn Center sees about 25 to 30 babies with the PNAC a year. None of these babies in the past five years have needed a liver transplant.
Charlie and Henry Fitzpatrick were two of those babies. The now 4-year-old twin boys were born prematurely at Texas Children’s Hospital Pavilion for Women and spent six months in the NICU. During their stay, both infants suffered from PNAC and were treated with Omegaven®. Since then, both their liver disease and intestinal failure have resolved. Charlie and Henry are now happy healthy preschoolers.
The twins’ mother, Aly Fitzpatrick, said Omegaven® played a big part in saving her children’s lives and that she is pleased to hear that the FDA approved the drug for use in babies like hers.
“The approval opens up a world of possibilities for these babies,” she said. “Now, more hospitals can embrace this without having to join a research study.”
Because of their experience with the drug, Texas Children’s is uniquely positioned to educate staff at other hospitals about the benefits of Omegaven® and train them on how to use it.
“It gives me great pride and satisfaction that we were part of this successful effort,” Premkumar said. “I would like to thank our dieticians, physicians, NNPs, pharmacists, nurses and of course, the babies and their families who supported us in this endeavor.”
Premkumar added that none of this would have happened if Dr. Steven Abrams and Keli Hawthorne, both former Texas Children’s staff, had not brought this project to the hospital.


























 When Kristine Hartin’s son was born almost a year ago, she was not prepared for the emergency cesarean section and almost four-week stay in the Neonatal Intensive Care Unit at Texas Children’s Hospital The Woodlands.
When Kristine Hartin’s son was born almost a year ago, she was not prepared for the emergency cesarean section and almost four-week stay in the Neonatal Intensive Care Unit at Texas Children’s Hospital The Woodlands.























 Hope Elizabeth Richards, one of the formerly conjoined twin girls separated at Texas Children’s earlier this year, was discharged April 25 after spending 482 days in the hospital. Hope joined her sister, Anna Grace, who was discharged on March 2.
Hope Elizabeth Richards, one of the formerly conjoined twin girls separated at Texas Children’s earlier this year, was discharged April 25 after spending 482 days in the hospital. Hope joined her sister, Anna Grace, who was discharged on March 2.







 Less than two months after being separated from her sister Hope in a seven-hour surgery at Texas Children’s Hospital, Anna Grace Richards got to go home.
Less than two months after being separated from her sister Hope in a seven-hour surgery at Texas Children’s Hospital, Anna Grace Richards got to go home.



