2020 has been an unprecedented year filled with many challenges. We’ve engaged in social distancing practices like we have never done before. We are wearing protective face masks, both at work and in public, in an effort to protect ourselves, each other, and prevent the further spread of the coronavirus.
But despite the uncertainty and daily disruptions caused by the COVID-19 pandemic, this health crisis has prompted our physicians, nurses and other patient care staff to explore innovative, non-traditional approaches to patient care processes – like e-rounding – to enhance the provider/patient experience.
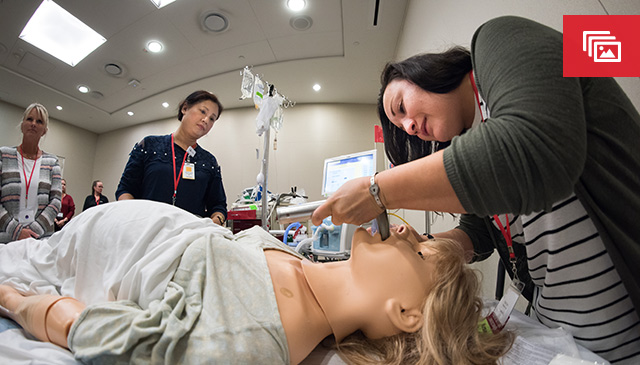
Daily patient rounding has been around for centuries, and is an important part of the patient care process. Before COVID-19, a group of multidisciplinary staff would gather in or outside a patient room to discuss the patient’s condition and plan of care with the patient’s family, taking into account the experience, concerns, questions and needs of the patient. Through this multidisciplinary, family-centered approach, each team member would then contribute their expertise to support the best possible care/outcomes for the patient.
To adapt to COVID-19 and to ensure social distancing practices are followed, our critical care teams began conducting patient e-rounding in April, which has been a beneficial change from the norm.
“E-rounding has been a big change for us,” said Dr. Jordana Goldman, attending physician in Critical Care. “Rounds are as old as time in medicine and so it takes a little bit of practice to get use to it. But once you get the flow of it, it really works well. Our physician and nursing leaders, and the e-Health and IS teams have been very supportive in helping us leverage new technology to make e-rounding possible.”
Through the VidyoConnect platform, virtual “rooms” are created that are then available for all rounding team members to join. During e-rounding, an attending physician, bedside nurse and family member, can be outside the patient’s room in front of a computer screen while maintaining social distancing, and can communicate virtually with remote team members including our consultants, the provider team (consisting of APPs, fellows and residents) dietitian, pharmacy, Respiratory Therapy support and other members.
“We facilitated the implementation of e-rounding by working with Dr. Goldman and Dr. Aarti Bavare to integrate their ideal workflow using the software and hardware that we already had available,” said Dr. Robert Ball, medical director of e-Health. “It was the team work of Information Services, e-Health and the physician champions that made it a reality. When you have amazing innovators in every corner of our organization working together to enhance this process, there are no obstacles that cannot be overcome.”
Since e-rounding was first introduced in the PICU and CICU in April, e-rounding has expanded to other parts of the hospital including the acute care cardiology floor. PHM has been working on the acute care side on a version of e-rounds to help with the education of the residents and medical students. Plans are underway to expand e-rounding capabilities to the Pavilion for Women and NICUs with the option of e-rounding being made available to all inpatient areas at our three hospital campuses in the coming weeks.
Our e-Health teams are also working on the ability to leverage VidyoConnect to communicate with families in a HIPAA compliant way so they can join rounds when they are not able to be at the bedside.
“The disruption of COVID-19 has allowed us to take a closer look at our rounding practices and see how we can improve them for our patients, team, learners and consultants,” Goldman said. “This is a very new process for us, but our team’s willingness to engage in this novel approach has been pretty phenomenal.”