Inclement weather update no. 3: Resuming normal operations
As of this afternoon, normal operations have resumed throughout the Texas Children’s system. Our clinics and primary care offices are now seeing patients during our regular hours and accommodating appointments that had to be rescheduled.
We want to thank all of you for carefully braving the weather to come into work yesterday and today. Your efforts to be here and your dedication to our patients ensured that we provided them safe, seamless care, and further demonstrate that we are an organization of staff and employees who think and act quickly and thoughtfully during times of challenge.
As we prepare for another deep freeze tonight, please be careful as you return home to your families. We encourage you to exercise caution when navigating roadways as some areas may still be wet or icy from earlier precipitation.
Judy Swanson
Administrator On Call
James Mitchell
Emergency Management
Inclement weather update no. 2: Tuesday, 2:15 p.m.
As expected, much of the Houston area is experiencing rain and below freezing temperatures. As we continue to monitor local reports, Texas Children’s leadership throughout the day has been assessing the needs and staffing of both patient care and non-patient-care areas within the hospitals, clinics, practices and health centers.
New information
- Inpatient operations. At this time, we are continuing operations as normal throughout the Texas Children’s system. Leaders will continue to assess staffing needs and will make adjustments accordingly. Staff who want to come in early prior to their shift should contact their leader. If you choose to spend the night, bring an overnight bag. Cots will be available for staff if you are unable to return home.
- Outpatient operations. We are planning to suspend outpatient services by 3 p.m. today. Outpatient clinics will open at 10 a.m. on Wednesday to allow patients and staff more time to arrive to their destination.
- Shuttles services from Garage 19 and Meyer to the Medical Center Campus are running on schedule.
- One-to-one handoff will occur in the inpatient areas at shift change
Medical Center campus retail food service
Tuesday
Food Court: closing early at 3 p.m.
Fresh Bistro: normal hours 6:30 a.m. – 3 p.m.
Coffee Corner: closing early at 9 p.m. (sandwiches, paninis, salads and soup) – usually stays open until 11pm
Wednesday
*This is the plan for now, although staffing could affect opening times
Coffee Corner: 6 a.m. – midnight
Fresh Bistro: 6:30 a.m. – 3 p.m. (will evaluate station closures based on staffing and volumes)
Food Court: 10:30 a.m. – 6:30 p.m. (will evaluate station closures based on staffing and volumes)
West Campus Retail Food Service
Tuesday
DOTS Kitchen – will remain open until 6:30 p.m., Deli window in DOTs will remain open until 8pm (EXTENDED HOURS).
Coffee Spot: Closes at 2:30 p.m. per normal operations.
Wednesday
*Planned to maintain normal hours, given that staff can arrive tomorrow morning safely.
Coffee Spot: will open at 6:30am
DOTS Kitchen: will open at 7am
Sleet and freezing rain are expected to create hazardous road conditions especially during the afternoon/evening commute. We encourage staff to exercise caution when navigating roadways especially on bridges and overpasses as water can freeze very quickly with a sudden drop in temperatures. Please plan for additional travel time, and be sure to communicate with your leaders should your arrival to work be delayed due to the inclement weather conditions.
We will continue to monitor the weather and assess any possible impacts to you, our patients and their families. and will send additional global alerts as needed. For more information, including the latest weather, traffic and road conditions, go to the Emergency Management Connect site and the National Weather Service website.
Judy Swanson
Administrator On Call
James Mitchell
Emergency Management
Inclement weather expected tomorrow: Monday, 9:30 p.m.
The National Weather Service is forecasting rain and below freezing temperatures across much of southeast Texas. Light rain is expected to begin at 2 a.m. on Tuesday. The morning commute is not expected to be affected. However, as temperatures begin to drop during the mid-morning hours, sleet and freezing rain could create hazardous road conditions especially during the afternoon commute.
We are monitoring local reports and will continue to do so throughout tonight and tomorrow morning. As of now, Texas Children’s is expected to remain fully operational. This includes both patient care and non-patient-care areas within the hospitals, clinics, practices and health centers. However, leaders are assessing the needs and staffing of their respective areas and will subsequently provide any further information or instruction.
We know staff and employees may be concerned about the impending weather conditions. Please remember that we all are here to take care of our patients, and ensuring that their care is safe and seamless is our priority. Please plan to get an early start tomorrow so you can make a thoughtful assessment of the current weather situation and your plans for reporting to work safely. We encourage you to exercise caution when navigating roadways and plan ahead in case there is an interruption to any city services or school closures.
For more information, including the latest weather, traffic and road conditions, go to the Emergency Management Connect site and the National Weather Service website.
Judy Swanson
Administrator On Call
James Mitchell
Emergency Management













































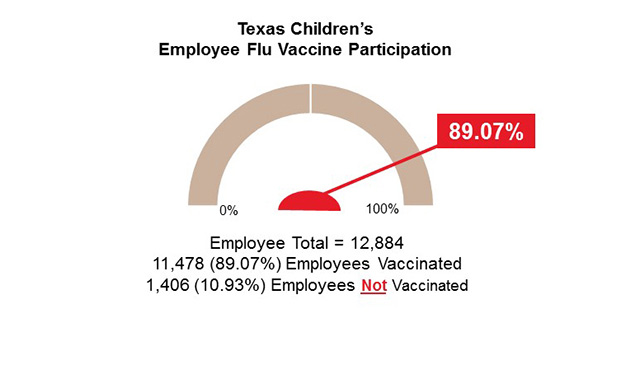 As of yesterday, 89 percent of Texas Children’s employees have received their flu shot. Last year, we achieved over a 90 percent vaccination rate, and this year, we want to beat that rate! We can do it! A special thank you to all of you for getting vaccinated!
As of yesterday, 89 percent of Texas Children’s employees have received their flu shot. Last year, we achieved over a 90 percent vaccination rate, and this year, we want to beat that rate! We can do it! A special thank you to all of you for getting vaccinated!






























