
Brittany Walters shares how she adapted her fitness routine to stay active and safe during COVID-19, and she hopes her story will inspire others to make their wellness a priority too. Read more

Brittany Walters shares how she adapted her fitness routine to stay active and safe during COVID-19, and she hopes her story will inspire others to make their wellness a priority too. Read more
As Hurricane Laura gained strength in the Gulf of Mexico and set its sights on landing as a Category 4 hurricane somewhere along the Texas/Louisiana coastline, Texas Children’s employees assigned to ride-out the storm at one of our three hospital campuses packed their bags and headed to their designated areas.
Just like they did three years ago when Hurricane Harvey was upon us and in years past when other storms were headed our way, they showed up to help take care of our patients and their families, even during a potential storm.
This year, with the COVID-19 pandemic still in our midst, there were additional concerns to tend to and plan for, but that didn’t deter anyone from showing up ready to carry out Texas Children’s mission of caring for children and women no matter what, under good circumstances and trying ones, too.
“Everyone’s attitude has been perfect,” said Susana De La Torre, whose job was to help direct people to and from their assigned sleeping quarters in Mark A. Wallace Tower. “No one has had anything negative to say.”
When leaders decided to active the organization’s ride-out team on August 26, the path of Hurricane Laura was still fluctuating with some forecasts pointing it right at Houston. Fortunately for our region, the storm ended up tracking east sparing us from the severe damage it dealt our neighbors. Nevertheless, we were prepared for the worst even during a pandemic.
To keep everyone safe while riding out the storm, everyone was required to adhere to all COVID-19 precautions and protocols, including screening upon arrival and every 24 hours thereafter, masking, socially-distant sleep accommodations, and dedicated areas for employees who begin to experience COVID-19 symptoms.
Employee Health was available throughout the ride-out if an individual exhibited symptoms of COVID-19 to help isolate them, monitor their symptoms, provide medical assistance and assess the need for COVID-19 testing. Had an employee’s medical condition required a higher level of care, there was a medical team on standby and our Employee Medical Clinic Physician was also available.
The departments of Organizational Resilience, Infection Control, Facilities and the Incident Command Planning Section worked on these plans for months and were prepared to implement them prior to everyone’s arrival.
Burt Gumeringer, senior vice president of facilities and operations, said leaders have been thinking for months about what it would look like to have employees come into the hospital and ride out a hurricane during a pandemic.
“Our primary concern was protecting our staff,” Gumeringer said. “The two main things we knew we had to change were sleeping arrangements and screening.”
Sleeping arrangements were made so that people were socially distant and a policy stating that employees on ride out had to be screened every 24 hours even if they didn’t leave the building was put into place.
Dr. Brent Kaziny, medical director of Emergency Management, said Texas Children’s has a duty to provide services to our patients and families during events such as these.
“In order to do that, we need to make sure our home is in order and that our families are in good hands so that we can come to the hospital and do what we need to do for those we serve,” Kaziny said. “Being prepared is of upmost importance.”
Hurricane season is not over yet. It won’t come to a close until November 30. So, we all have to stay vigilant and aware of storms brewing in the Atlantic. Pay close attention to local media reports concerning weather conditions and make sure you stay up to date with Texas Children’s Emergency Management communications. These are sent via texts, phone calls and emails through the Texas Children’s Notification System. Please make sure to update your personal information in MOLI with your current mobile phone number so you receive all messages in a timely manner. Here are the instructions for updating your information in MOLI.

On the 15th anniversary of the devastating storm, Dr. Brent Kaziny recalls in a TMC News story his experience as a young intern in New Orleans during Hurricane Katrina and how it shaped his career in emergency management. Read more
Each year in September, Texas Children’s Cancer Center goes gold to honor the courageous journeys of our patients and families who have been touched by pediatric cancer and to create awareness about the challenges these children and their loved ones face. It’s also a special time to honor our Cancer Center staff and everyone who plays a role in ensuring that our patients and their families get the care and support they need.
This year, awareness celebrations will be conducted differently to maintain social distancing due to the COVID-19 pandemic. We will celebrate with our families and staff in a virtual way, instead of the large celebratory gatherings across our four campuses (Main, West, Woodlands and Vannie Cook) that we have held in previous years.
“Despite the challenges we all face due to COVID-19, we have a phenomenal team of providers who will do whatever it takes 24/7 to ensure our patients and their families get the care and treatment they need,” said Dr. Susan Blaney, director of Texas Children’s Cancer and Hematology Centers. “Our Cancer Center helps children fight and defeat cancer every day. We hope you will stand with us in Going Gold for childhood cancer, so that together, we can create a healthier future for these children who need our care.”
In this video spotlight on Texas Children’s Cancer Center, Blaney shares how our teams are advancing science and research every day to find cures and give hope to the many patients and families we serve.
Throughout September, Texas Children’s Cancer Center encourages staff to participate in several virtual activities to help shine the light on childhood cancer.
Patient Activities
The Cancer and Hematology Centers’ inpatient team is hosting a carnival and the outpatient team is hosting a variety of activities throughout the month to honor childhood cancer awareness month as well as the patient populations impacted by the diseases/disorders being honored in September.
Childhood Cancer Awareness Month
September 17: Houston City Hall lights up in Gold
Click here to learn more about Texas Children’s Cancer.

Approximately 25 percent of children and adolescents in the United States have a diagnosed mental, behavioral, learning, or developmental disorder, and these numbers are growing rapidly as more children and families continue to be impacted by the uncertainty, economic stress and daily disruption caused by the COVID-19 global pandemic.
“Since we began building our developmental-behavioral health infrastructure in The Woodlands in 2016, our focus has been on developing a robust program that serves the broad developmental and mental health care and behavioral needs of children and families,” said Dr. Paul Sirbaugh, chief medical officer at Texas Children’s Hospital The Woodlands. “From diagnosis to a multidisciplinary treatment approach, our patients and families can access services in their own community from behavioral health specialists who treat a myriad of mental health issues.”
The Developmental-Behavioral Health team consists of psychiatrists, psychologists, a clinical social worker and a developmental-behavioral pediatrician who collaborate with colleagues at Texas Children’s, Texas Children’s Pediatrics and in the community to design efficient methods to screen and identify patients in need of our services.
Having developmental-behavioral health services available at Texas Children’s provides the security of knowing that children and families will benefit from science-informed practice and a focus on quality and outcomes, ensuring our patients and their families have access to the right care, in the right place at the right time.
Referrals to the Developmental-Behavioral Health team at The Woodlands are routed through the Behavioral and Developmental Sciences Referral Center. A dedicated referral team reviews all patient referrals closely and triages them to the appropriate service, location and provider based on the patient’s needs. The developmental-behavioral health providers can also bring other members of the team on board for those patients who would benefit from more than one service.
The psychology team in The Woodlands offers diagnostic assessment and psychotherapy intervention services either through in-person or e-Health video visits for children and adolescents with behavioral health concerns.
“Within psychology, our focus is on using evidence-based tools and interventions to diagnose, treat and monitor outcomes for our patients,” said Chief of Psychology Dr. Karin Price. “Our psychology providers work with a broad spectrum of pediatric and adolescent patients including those with common mental health concerns and difficulties related to acute and chronic health issues.”
The Woodlands team consists of four psychologists and a certified social worker with diverse specialties:
While psychologists and psychiatrists both specialize in evidence-based diagnostic assessment and treatment planning for patients, Texas Children’s psychiatrists provide more specialization in medication management.
Under the guidance of Dr. Kirti Saxena, interim section chief of psychiatry at Texas Children’s, the psychiatry team in The Woodlands consists of two psychiatrists Drs. Nabil Guirguis and Humera Danwar, who also see patients through in-person visits or e-Health video visits, making it easier for providers and their patients to connect remotely.
“We have a full case load of patients in our clinic,” said Saxena. “There is a huge demand for children with primary psychiatric needs, but also patients with chronic medical conditions who need psychiatric services. Many of our slots are filled for existing patients, so trying to get new patients in has been challenging for us, but our providers are doing a fantastic job of accommodating as many patients as we can given our current resources.”
Often times, patients with mental health needs may benefit from more than one service. If a patient has been diagnosed with a mood or anxiety disorder, a traumatic brain injury, or is lagging behind in school after a diagnosis of Attention-Deficit/Hyperactivity Disorder (ADHD) – and in addition to psychotherapy – they need medication to manage the symptoms of their illness more effectively, that’s when the expertise of psychiatry comes into play.
“We collaborate with our psychology partners regularly to ensure that we provide the most comprehensive, individualized treatment plan for our patients,” said Danwar. “We also work with colleagues in developmental pediatrics. If we have a patient with autism whose symptoms are not being managed well with other therapies, and medication management is needed, that’s when my expertise is needed to assist with their treatment plan.”
The Meyer Center for Developmental Pediatrics at Texas Children’s is the third component of the comprehensive model of care for patients and their families enrolled in the Developmental-Behavioral Health Program in The Woodlands.
Led by Dr. Robert Voigt, the chief of service for the Meyer Center and head of the section of developmental pediatrics in the Department of Pediatrics at Baylor College of Medicine, our developmental-behavioral pediatricians provide medically directed diagnostic consultations for infants, children and adolescents spanning the full spectrum of developmental-behavioral pediatrics – from intellectual disabilities, autism spectrum disorders, and cerebral palsy to learning disabilities, attention-deficit/hyperactivity disorder (ADHD), and motor coordination disorders. The Meyer Center also provides medically directed developmental evaluations for children at increased risk for developmental-behavioral disorders due to prematurity or other neonatal complications, medical conditions such as congenital heart disease, genetic syndromes, or neurologic disorders, or adverse psychosocial experiences.
“Our approach is interdisciplinary and family-centered, and our evaluation considers the individual and collective impact of biological, genetic, environmental and social factors,” said Dr. Candice Allen, the only developmental- behavioral pediatrician at Texas Children’s Hospital The Woodlands. “Our team evaluates each child and works with the family on assessments, team meetings and conferences to develop an individualized treatment program so that every child who seeks our services receives the care and support they need to achieve their highest potential.”
As medical director of the SOAR (High Risk Neonatal Follow Up) Program at The Woodlands, Allen works closely with families to ensure a seamless transition of care following their infant’s discharge from the NICU. Through this program, the infant’s early growth and development are tracked to ensure that any developmental concerns are detected and addressed as early as possible. If developmental concerns arise, The Woodlands team of SOAR Occupational, Physical and Speech therapists are ready and able to provide any therapy services that are needed.
“It’s so critical that our patients are able to readily access all of our developmental-behavioral health services in The Woodlands,” Allen said. “The sooner that a patient’s mental health, neurodevelopmental and/or neurobehavioral concerns are diagnosed and treated early on, the better the long term outcomes will be for the patient and their family.”
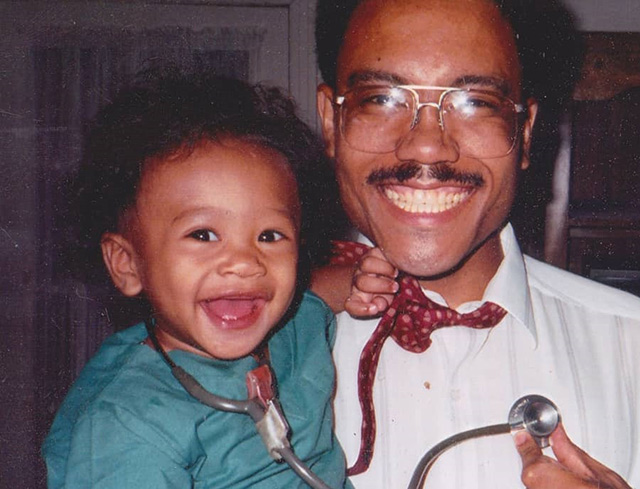
Pediatric Surgeon Dr. Paul Minifee has worked at Texas Children’s for almost three decades. Over the years, one of his primary focuses has become educating and mentoring residents and medical students on rotations in pediatric surgery.
“I have always enjoyed sharing my knowledge and experience with others, especially young people who are early in their medical careers,” Minifee said. “It’s been one of the most fulfilling parts of my career.”
Recently, Minifee got the opportunity to teach and operate with a very special student – his son, Dr. Chris Minifee, a third-year surgical resident at the University of Texas Medical Branch. Chris is spending two and a half months at Texas Children’s on rotation with the Orthopedic Surgery Department.
The day he collaborated with his dad in the operating room he was performing an anterior scoliosis repair with Dr. Brian Smith, Texas Children’s chief of orthopedic surgery. Paul came in at the beginning and the end of the surgery to open and close the patient’s chest. Chris assisted him with the procedure, a common practice for orthopedic surgeons in cases such as the one they were working on.
“I immediately went to the coaching skills I learned in baseball,” Paul said about how he handled guiding his son in the operating room. “They worked back then and they seemed to work that day too.”
Paul said his son did a great job and that he executed his part of the procedure very well. What made him most proud was the positive comments from his colleagues about his son’s work in the operating room that day and on other occasions during his rotation.
“It was truly a joy to be there with him and to hear from others what good work he’s doing for others,” Paul said. He added that the father-son duo was making history that day in that he, the first Black pediatric surgeon trained in Texas and the second to be licensed in the state, was operating with his son, who is one of a small but growing number of Black surgeons in the state and the nation. “We were making history in there,” Paul said. “I’m glad it was at Texas Children’s, a place where I have always felt comfortable, accepted and able to grow in my career.”
Chris said operating with his dad has thus far been the proudest moment of his medical career. The operating lounge they were in after surgery, Chris said, was the same lounge he saw his dad in years ago when he shadowed him during junior college. It was around then that he decided to pursue medicine instead of his first love – baseball.
“I wanted to be a professional baseball player but that didn’t pan out,” Chris said. “I’m glad I had a backup plan (orthopedic medicine) and that I have come to love it as much as or more so than baseball.”
Chris said a lot of what his dad taught him on the ballfield translated over to the classroom and now the OR. Some of those things include team work, persistence, and the desire and drive to be your best.
Throughout his rotation at Texas Children’s and from what he’s seen and heard through his dad over the years, Texas Children’s is a place where people’s best is exhibited across the board. He said that includes diversity among the organization’s workforce.
While operating at Texas Children’s, Chris said, the OR has been filled with people from different ethnicities and walks of life. “You probably didn’t see that 20 years ago, but things have changed, which is refreshing.” he said.
Volunteer Services hosted several events last week for employees to make face buttons. The buttons worn by employees are intended to help put patients at ease, as they give them a glimpse of the smiling Texas Children’s face beneath the ‘ll and other personal protective equipment.