 At Texas Children’s, we feel strongly that it is our responsibly to educate patients about the health plans we are in network with and how they can access our expert care. Therefore, we want to make sure Amerigroup members are aware that Texas Children’s is not a participating provider with Amerigroup. Those patients have the right to change health plans to ensure continuity of care.
At Texas Children’s, we feel strongly that it is our responsibly to educate patients about the health plans we are in network with and how they can access our expert care. Therefore, we want to make sure Amerigroup members are aware that Texas Children’s is not a participating provider with Amerigroup. Those patients have the right to change health plans to ensure continuity of care.
Amerigroup currently insures 9,500 past and present Texas Children’s patients under Amerigroup STAR, Amerigroup STAR Plus, Amerigroup STAR Kids, or Amerigroup Children’s Health Insurance Program (CHIP) plan.
To make sure these patients receive uninterrupted access to care at Texas Children’s, we are recommending they change their coverage to a health plan that Texas Children’s is in-network with. As an eligible STAR, STAR Plus, STAR Kids, or CHIP plan member, they have a choice in the plan they select for coverage. They also have the right to change plans.
“We have been treating these patients out-of-network for the past five years hoping Amerigroup would work with us to either become an in-network provider or educate their customers about the options available to them,” said Kabby Thompson, director of managed care contracting. “It is clear that’s not going to happen. We feel it is in our patients’ best interest to educate them about the plans we are in network with and to help them transition into an in-network plan if that’s how they want to move forward.”
A similar plan of action worked well last November when Texas Children’s became an out of network provider to 6,000 Molina members. More than half have switched to an in-network plan.
A letter has been sent to patient families who have been a Texas Children’s patient within the past year and whose records say they are covered by Amerigroup. Depending on your role at Texas Children’s, you could receive questions from patient families and others about this change. Below is information to help you answer those questions and to places to direct people if you cannot.
“We appreciate your help in getting these patients and families the help they need,” Thompson said. “Their health care is important to us.”
Click here to access the information below and more.
How can Amerigroup patients and families change their health plans?
For Amerigroup STAR, Amerigroup STAR Kids and Amerigroup STAR Plus members: The Texas Medicaid program allows people to change their or their child’s health plan.
- Patients and their families can learn more by calling the Texas STAR Program Helpline at 1-800-964-2777.
- Patients and families can request to change their health plan at any time for any reason. If they call to change their health plan on or before the 15th of the month, the change will take place on the first day of the next month.
- If they call after the 15th of the month, the change will take place the first day of the second month after that. For example:
- If they call on or before October 15, their change will take place on November 1.
- If they call after October 15, their change will take place on December 1.
For Amerigroup CHIP members: The Texas Medicaid program allows patients and their families to change their or their child’s health plan.
- Patients and families can learn more by calling CHIP toll-free at 1-800-647-6558.
- During the first 90 days after they or their child are enrolled in a health plan, they can change to another plan once for any reason.
- If they show good cause, they can also change health plans at any time. An example of “good cause” is when they or their child can’t get the care you need through the health plan. An inadequate network or a change in the network status of their treating provider is also considered “good cause.”
- They can also change health plans during the annual CHIP reenrollment period.
The Texas Medicaid program allows patients and families to change their or their child’s health plan every 30 days. They can learn more about how to do this and begin to make the change by calling the Texas STAR Program Helpline at 1-800-964-2777 (STAR or STAR Plus) or CHIP toll-free at 1-800-647-6558.
Questions patients and families might have about care at Texas Children’s:
As an out of network member, will patients still be able to receive care at Texas Children’s Hospital?
Rescheduling: In cases where Amerigroup has not responded to requests for both out-of-network authorizations and Single Case Agreements before the scheduled visit, Texas Children’s will contact patients/their families before their scheduled visit to reschedule once Amerigroup has responded.
Emergency Medical Care: Amerigroup advises that you go to an in-network provider for emergency care. Texas Children’s Hospital will treat children in the event they have an emergency. If a child is seen in the Emergency Center for emergency care, the medical team will work with the patient and their family to decide how to provide care after the doctor’s medical evaluation. Amerigroup will help find follow up care with a provider who is in network.
Urgent Medical Care: In order to receive urgent care at a Texas Children’s Urgent Care location, Amerigroup must approve an out-of-network authorization. This could be difficult because of the urgent nature of a patient’s condition and the time it takes to get an authorization. Amerigroup may also redirect care to another in-network provider.
Routine Care: In most cases, Amerigroup will require patients and their families to receive routine or urgent care from a network provider. In order to receive care at Texas Children’s, Amerigroup must approve an out-of-network. Amerigroup may also redirect care to another in-network provider.
Who should I contact if I have further questions?
If you want to learn more about changing your or your child’s health plan, you can call the Texas STAR Program Helpline at 1-800-964-2777 or CHIP toll-free at 1-800-647-6558.
If you have questions for Amerigroup, you may call their Member Services department toll-free at 1-800-964-2777. If you are not satisfied with the response from Amerigroup, you can contact the Texas Health and Human Services Commission (HHSC) by calling toll-free 1-866-566-8989.
If you have questions for Texas Children’s Hospital or Texas Children’s Physician Services Organization, you may call us at 832-824-1000 Monday through Friday from 8 a.m. to 5 p.m. Central time. Texas Children’s Pediatrics can be reached at 832-824-2999.
What Medicaid Health Plans is Texas Children’s in-network with?
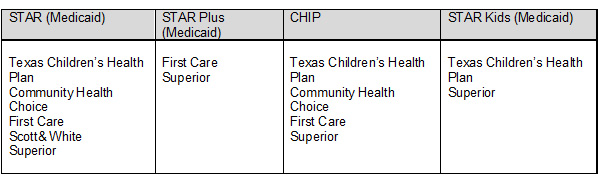
Texas Children’s Hospital and Texas Children’s Physician Service Organization are in-network with the following Medicaid Health Plans
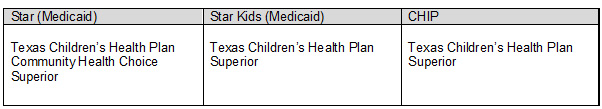
Texas Children’s Pediatrics is in-network with the following Medicaid Health Plans





















 On June 18, Texas Children’s Pediatrics opened its first primary care site in Austin, marking another milestone in Texas Children’s path toward creating a network of quality pediatric care for children and families living in the state’s capital city.
On June 18, Texas Children’s Pediatrics opened its first primary care site in Austin, marking another milestone in Texas Children’s path toward creating a network of quality pediatric care for children and families living in the state’s capital city. In an effort to better serve patients seeking care at one of 10 Texas Children’s Urgent Care sites, wait times for each location have been posted on the Urgent Care website.
In an effort to better serve patients seeking care at one of 10 Texas Children’s Urgent Care sites, wait times for each location have been posted on the Urgent Care website.








