As one of the best pediatric cancer centers in the nation, experts at Texas Children’s Cancer Center are on the forefront of cutting-edge basic, translational and clinical research. The center’s world-renowned faculty have pioneered many of the now standard protocols for treating and curing children with cancer.
Scientists and clinical experts at the center are conducting more than 250 clinical trials – more than the majority of pediatric cancer centers in the nation. In addition, the center’s Developmental Therapeutics Program and its Cell and Gene Therapy Program have been leaders in the study of novel agents and immunotherapies, respectively, for the treatment of childhood cancer.
“Our physicians employ evidence-based guidelines and the most advanced clinical trials in the delivery of oncology care,” said Cancer Center Director Dr. Susan Blaney. “Our vast expertise in the development of new therapeutics means our patients have access to the most advanced and innovative therapies.”
Dr. Andras Heczey, one of the Cancer Center’s physician scientists and a member of the newly-formed Sky High Immunotherapy Center, is working with colleagues in his laboratory to develop novel treatments for children with solid tumors. His work is a prime example of what the Cancer Center is doing to advance treatments and ultimately find a cure for a disease that remains the leading cause of non-accidental death in children.
In honor of National Childhood Cancer Awareness Month, we interviewed Heczey about his research and why he thinks such work is so important to enhanced patient care.
What is the focus of your research?
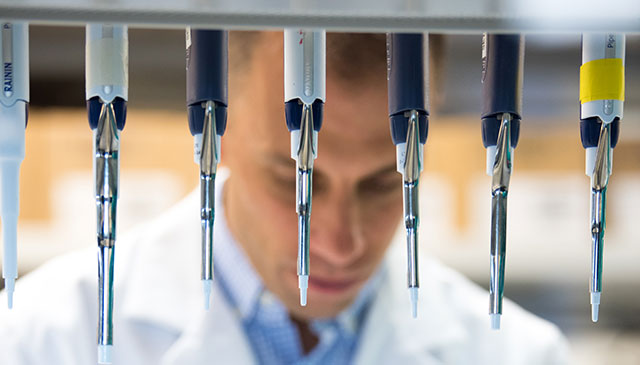
My research focuses on redirecting the normal immune system to attack cancer cells. T cells are a type of white blood cell that participate in the immune response. I am using genetically engineered T cells to treat liver tumors in children and Natural Killer T (NK-T) cells to treat neuroblastoma, a childhood tumor that most commonly involves the adrenal gland.
How exactly does this work?
We take patients’ white blood cells from a simple blood draw, modify them in the test tube to recognize and kill tumor cells, and then re-infuse these genetically engineered (modified) cells into the patient’s blood stream. The idea is that we train the immune system to kill the cancer cells. In patients with neuroblastoma, we modify Natural Killer T cells to express a protein called chimeric antigen receptor (CAR for short) that targets GD2, a molecule on tumor cells but not on normal tissues. When the Natural Killer T cells arrive at the neuroblastoma tissue, they recognize the GD2 molecule and kill the cancer cells. In liver cancer patients, we are using a similar strategy using T cells that express CAR targeting a molecule called Glypican-3, which is primarily expresses on liver cancer cells.
Have you used these treatments in children at Texas Children’s?
Last summer, we started our first human clinical study in children who have relapsed or have refractory high-risk neuroblastoma. So far, three children have been treated. The results we have observed thus far are very promising. We also have started our first human clinical study in children with relapsed or refractory liver cancer. The first patient was recently treated and we are eagerly waiting for the results.
What else are you studying in your laboratory?
In addition to developing strategies to kill the tumor cell, we are also closely studying the tumor environment. We know that when genetically engineered cells enter the tumor, the cancer cells and other cells within the tumor will fight back. We don’t really know how this happens. We have some ideas, but we and others in the field are closely evaluating what happens in human tumors after the engineered cells are infused. This is really important because we want to make sure our cell therapies are effective and that the responses are sustained and the patients are cured. Ultimately, we’ll also need to develop techniques to engineer the cells inside the body. Right now, we have to grow and test the cells before infusing them into the patient. This typically takes four to six weeks, depending on the product and how many cells needed to be manufactured. A patient cannot always wait that long. In the future, we envision strategies where a patient’s immune cells are engineered inside their body to quickly redirect them against the growing tumor cells.
Are you encouraged by what you are finding?
Yes, I am very encouraged. We are getting closer each and every day to finding a cure for some forms of childhood cancer.
Click here to view a preview of the next installment of “This is Cancer: Reflections from our patients.” This installment focuses on Tajah, who was diagnosed with osteosarcoma after visiting Texas Children’s Emergency Center with intense knee pain. The 13-year-old had to have her knee and femur removed. Surgeons replaced them with a metal extendable one, which will prevent her from undergoing several additional surgeries as she grows. The “This is Cancer” series documents the journeys of several families receiving care at Texas Children’s Cancer and Hematology Center. Their stories illustrate in intimate detail what they’re experiencing and how to better support them. Click here to learn more.