Like most parents, the Harts were nervous about their 10-month-old son’s surgery scheduled with Texas Children’s Division of Urology. In addition to regular jitters, they were especially concerned about their son undergoing general anesthesia.
“My husband did some research and found that it can be dangerous for young children,” Kayla Hart said. “So, needless to say, we were a little worried.”
Those worries were put to ease when their son’s pediatric anesthesiologist, Dr. Kevin Chu, and surgeon Dr. David Roth, explained the information the couple found online and offered another option, spinal anesthesia. Spinal anesthesia, numbs the lower part of the body to block pain versus general anesthesia, which puts a patient to sleep.
Texas Children’s Department of Anesthesiology and Department of Surgery recently started offering spinal anesthesia, when appropriate, to parents of young children. Rowan Hart was one of the hospital’s first patients to receive spinal anesthesia as an alternative to general anesthesia.
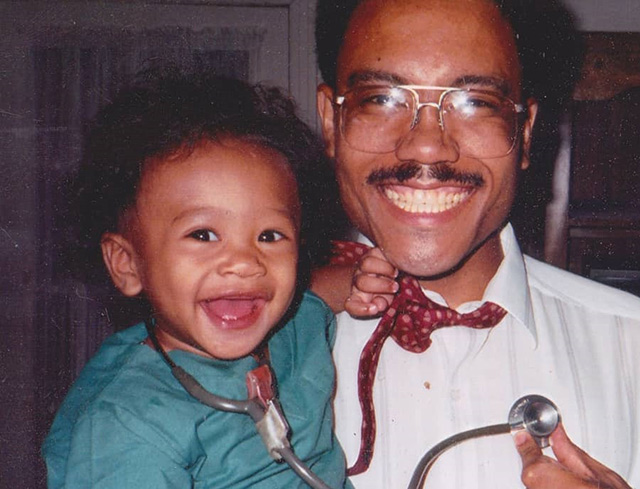
“When I went back to recovery, he woke up from the nap he was taking throughout surgery and was totally normal,” Hart said. “He wasn’t groggy at all and was even smiling.”
General Anesthesia Division Chief Dr. Olutoyin Olutoye said spinal anesthesia is a safe alternative to general anesthesia in patients under one year of age who are having surgery on the lower part of their body. She said if needed, the patient may receive a light sedative to make them relax but otherwise, they are awake during their procedure. There is no need for a breathing tube when a child receives spinal anesthesia and patients, like Rowan Hart, are alert and in good spirits post operatively.
“Even though anesthesia is much safer today than ever before, every anesthetic exposure and surgical encounter, has an element of risk and we must remain vigilant about communicating such risks to our patients and their families,” Olutoye said. “Offering an alternative to general anesthesia when appropriate is another way we can serve our patients and families in this capacity.”
On December 14, 2017, the U.S. Food and Drug Administration (FDA) released a drug safety communication about prolonged or repeated anesthetics in young children and pregnant women in their third trimester.
The FDA’s communication states:
- A single, short exposure to anesthesia appears to be safe.
- There is some evidence that longer (>3 hours) or repeated exposures could have negative effects on behavior or learning.
- Much more research is needed.
As a result of the communication Texas Children’s Hospital changed its anesthesia practice and started discussing the warning before surgery with the parents of all children 3 years of age and younger.
In addition, Texas Children’s Hospital adopted the warning’s recommendation that a discussion occur among parents, surgeons, other physicians and anesthesiologists about the duration of anesthesia, any plan for multiple general anesthetics for multiple procedures, and the possibility that the procedure could be delayed until after 3 years of age. Parent-education materials that cover these topics are available to our patients and their families.
“I think offering spinal anesthesia is another way we can remain on the leading edge of this issue,” said Roth, who helped spearhead the use of spinal anesthesia together with the Department of Anesthesiology, and who has operated on the patients who have received it thus far. “It’s a safe alternative that we can use to reduce any potential risks of general anesthesia in our younger population.”
Anesthesiologist-in-Chief Dr. Dean B. Andropoulos agreed and said the benefits of anesthesia must always be weighed against the risks of anesthesia itself and Texas Children’s does a good job at doing that.
“We are very serious about educating our patients and families prior to surgery about any risks and any options that can be taken to mitigate such risks,” Andropoulos said. “Using spinal anesthesia is a nice addition to what we already are doing to mitigate potential risk.”