Texas Children’s Hospital and Baylor College of Medicine launch a new clinical genomic sequencing program to help patients with undiagnosable conditions. Read more
Texas Children’s Hospital and Baylor College of Medicine launch a new clinical genomic sequencing program to help patients with undiagnosable conditions. Read more

Every day we make the impossible possible by doing things differently. Click here to see it again.

Mary Gordon shares an exciting opportunity for clinical staff nurses thanks to a generous gift from Mary Jo Andre and her husband, David, that will support nursing research now and in the future. Read more
More than 100 team members in Texas Children’s Department of Pathology were recently awarded the G.J. Buffone Pathology Improvement Award for the way they responded to the COVID-19 pandemic over the last year – extending shifts, adjusting schedules and making personal sacrifices to manage significantly increased volumes of testing in the lab.
Since March 2020, Pathology has received and tested more than 183,000 samples for COVID-19 diagnostic testing alone. This includes testing of Texas Children’s patients and team members, as well as patients from other hospitals in the Houston area. It is also in addition to various other tests needed for patient management and treatment of COVID-19, which caused test volumes in some specialties to rise dramatically.
For the diagnostic testing, technicians looked at samples like nasopharyngeal swabs, nasal/nasopharyngeal washes and bronchoalveolar lavages. Labs involved in this work included Specimen Management, which receives all specimens from various collection sites; Medical Microbiology & Virology, which handles rapid COVID-19 testing; and Molecular Microbiology, which handles both routine and rapid COVID-19 testing. Additional testing labs included Chemistry for COVID-19 antibody testing, and the Microbiome Center for COVID-19 sequencing for variant surveillance.
To accommodate the increased laboratory workload, Pathology team members worked tirelessly behind the scenes, stepping up to cover extra weekends and even eschewing family and personal time to remain flexible through inconsistent shifts in schedules. In some services where staffing has had to nearly double to keep up with the pace, leaders have managed their teams while also onboarding new technologists to meet the demand.
With a mission to provide state-of-the-art diagnostic services to Texas Children’s patients and their families, Pathology is committed to providing answers to support accurate diagnoses by obtaining puzzle pieces in the form of patient samples. The team celebrated National Medical Laboratory Professionals Week from April 19-23.
For a look at our Texas Children’s lab technicians – truly among the unsung heroes in health care – at work, check out the video above.
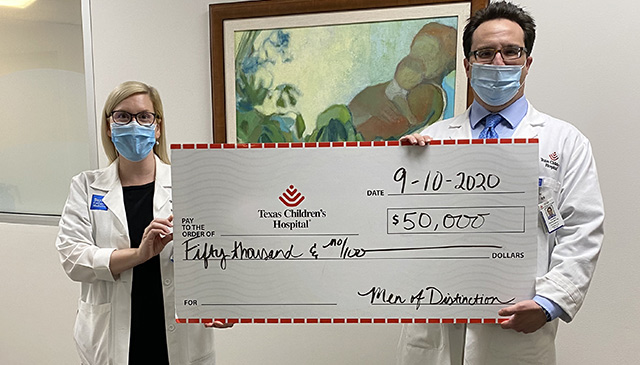
Men of Distinction (MOD) donated $50,000 to Texas Children’s to further research by Drs. Amy Hair and Geoffrey Preidis that focuses on developing new therapies for premature infants with liver and intestinal challenges while optimizing their overall nutrition and growth. This funding will enable Drs. Hair and Preidis to move forward with the initial sample analysis and position them well for future potential grants from the NIH.
Even though the 2020 Men of Distinction Luncheon fundraiser was postponed until later in 2021 due to COVID-19, organizers went ahead and awarded partial funding so that research can progress. Texas Children’s anticipates receiving the other half of the funding after the event.
Men of Distinction was founded in 2007 to support superior biomedical research, education, and patient care focused on pediatrics in the Texas Medical Center, which directly benefits the Houston community.
Since 2014, Men of Distinction has donated $400,000 to benefit pediatric research at Texas Children’s Hospital. Past awardees include:
2018:
Dr. Sanjiv Harpavat
Dr. Mary Elizabeth Tessier
2017:
Dr. Michael A. Belfort
2014:
Sundararajah Thevananther, Ph.D.
Dr. Richard Kellermayer

Calling all innovators! The Southwest National Pediatric Device Innovation Consortium (SWPDC) needs your help in identifying pediatric device projects that support COVID-19 related and other critical need projects.
SWPDC is a multi-institutional consortium supported by a U.S. Food and Drug Administration (FDA) P50 grant and anchored by Texas Children’s Hospital and Baylor College of Medicine that is dedicated to improving children’s health by supporting pediatric device innovators to create novel pediatric medical devices with local, regional, and national institutional and innovation partners.
The consortium is receiving supplemental funding to be able to award $100,000 in SWPDC 2020 Impact Grants for COVID-19 and other critical needs areas in the form of seed grants or in-kind support for related pediatric device projects. Applications are being accepted from July 8 through August 5. All pediatric device innovators can apply.
“Across the country, entrepreneurs are pivoting to address the health care challenges of the COVID-19 pandemic,” said Dr. Chester Koh, executive director and contact PI of SWPDC, Texas Children’s pediatric urologist, and Baylor Professor of Urology, OB/GYN, and Pediatrics. “This is a great opportunity to be part of this effort, especially as children are increasingly recognized as a vulnerable population for COVID-19.”
Interested applicants should complete the application here. The application consists of a short questionnaire, an itemized budget (up to $25,000 max) and an optional, but highly encouraged, one- to two-minute video pitch. Further information may be requested by the SWPDC staff, and funding will be made available September 1.
In this rapid cycle opportunity, these grants will be awarded to pediatric device companies as seed funding or in-kind services to support activities that improve the health care of the pediatric community during this pandemic. This opportunity is nonexclusive to COVID-19 and can also apply to other critical needs areas such as addressing the opioid epidemic. Medical devices with adult indications that are expanding their focus to the pediatric population are also welcome to apply.
Examples related to COVID-19:

The rapid spread of COVID-19 has resulted in more than 4 million cases worldwide. The disease has a marked preference for adults with children being relatively spared. Understanding this preference might hold the key to the identification of therapeutic targets and is the topic of a paper Texas Children’s, Baylor College of Medicine, University of Texas Health Science Center and University of Texas McGovern Medical School physicians recently published in The American Journal of Physiology-Lung Cellular and Molecular Physiology.
The paper suggests differences in lung physiology and immune function as possible reasons why children are often spared from severe illness associated with SARS-CoV-2, the novel coronavirus that causes COVID-19.
The number of children under the age of 18 infected with SARS-CoV-2 has been found to be considerably lower than adults. Early reports from China and Italy have shown that children who become infected with the virus show symptoms less often than adults and even when they are symptomatic, are less likely to develop respiratory symptoms such as a cough or shortness of breath. In most cases, the infected under-18 population does not become as severely ill as their older counterparts. The newly identified multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19, though serious, affects only about 1 percent of young people exposed to SARS-CoV-2.
“These profoundly decreased rates of symptomatic infection, hospitalization and death are well beyond statistical significance, require further examination and may hold the key to identifying therapeutic agents,” said the paper’s lead author, Texas Children’s Neonatologist Dr. Krithika Lingappan.
The way the SARS-CoV-2 virus enters the body and the state of the immune system itself are thought to be two primary differences in how children and adults become infected with the novel coronarvirus.
SARS-CoV-2 enters the body by binding to angiotensin converting enzyme-2 (ACE2), an enzyme that is attached to the outer surface of cells in the lungs, arteries, heart and other organs. This interaction is analogous to the virus unlocking the door to a cell. The higher the expression of ACE2 in the body, the more likely the virus will get in.
Studies have found that expression of ACE2 in the lungs increases with age. Infants and very young children have very low ACE2 expression, and older children still have lower expression than adults. Research suggests that children may be protected from the serious respiratory components of COVID-19 — including acute respiratory distress syndrome — due to their reduced ACE2 expression.
The immune system also plays a role in the novel coronavirus infection. Heightened immune response is often a factor in the inflammatory “cytokine storm” phase of COVID-19, in which the body attacks itself. Studies have found that CD4+ fighter cells in the immune system play an important role in limiting replication of the virus and that adults with moderate-to-severe COVID-19 had lower levels of CD4+ and CD8+ cells. Lung tissue in children naturally has a higher concentration of regulator T-cells, which may protect against severe COVID-19 by suppressing the immune response that, in adults, may lead to a cytokine storm.
“Selective, age-associated mortality render[s] COVID-19 a unique, infectious disease,” said Texas Children’s Neonatologist and Dr. Jonathan Davies, another author of the paper. “Insights into age-related variability in pathophysiological processes may offer critical observations, revealing focused paths of therapeutic investigation.”
Davies and Lingappan both said multidisciplinary collaboration between physicians and scientists, engaged in both pediatric and adult pursuits, holds significant promise and should be encouraged.
Click here to read the full article, “Understanding the age divide in COVID-19: Why are children overwhelmingly spared?”
Authors of the paper are:
Dr. Krithika Lingappan, Texas Children’s and Baylor College of Medicine
Dr. Harry Karimouty-Quintana, University of Texas Health Science Center
Dr. Jonathan Davies, Texas Children’s and Baylor College of Medicine
Dr. Bindu Akkanti, University of Texas Health Science Center
Dr. Matthew Harting, University of Texas Health Science Center