When the Texas Children’s project team started the journey to implement the Epic software system 15 years ago, they didn’t expect to change the landscape of pediatric health care, but they did just that. Our strategy proved to be the winning formula for integrating the software system in to pediatric health care operations, and we became the Epic best practice for the industry.
“The project team set out with a goal to ensure our version of Epic would be a game changer for our patients, staff and Texas Children’s, and they certainly delivered,” said Teresa Tonthat, vice president, Information Services. “I’m so proud of what we’ve accomplished together and what we’ve developed for our staff, patients and other health care professionals. This is an important milestone to take time and celebrate, but we have no plans of stopping. I’m excited for what comes next.”
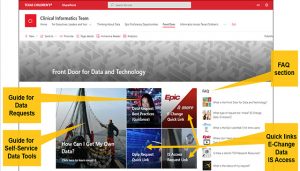
Together, our IS and clinical teams approached the implementation with a goal to provide a best-in-class software platform tailored to fit the specific needs of our staff and patients. The result was a comprehensive resource with the right tools to help us provide more thorough and efficient care for our patients.
“Nurses are dedicated to providing the highest quality, safest care possible to our patients. We must be up to speed at all times with accurate information at our fingertips. Having the right information available from one source at bedside has been a huge advantage,” Jennifer Sanders, vice president and associate chief nurse executive. “Epic helps us be more efficient, better informed and in the best position to deliver exceptional care to our patients.”
The Epic system is comprised of 54 modules our clinical teams use to help them make informed decisions on patient care. There are a handful, which have had the biggest impact, including:
- MyChart Patient Portal. Allows patients to access their medical records, schedule appointments and communicate with their doctors online. It’s help make it easier for patients to be involved in their own care and have a better understanding of their health.
- Mobility. Epic Rover has become an indispensable tool for healthcare professionals, particularly nurses, in various clinical settings. By providing secure and mobile access to patient information and streamlining critical processes like medication administration, specimen collection and infusion pump management, Epic Rover enhances patient safety, reduces errors and improves the efficiency of healthcare delivery.
- Interoperability. This has allowed different healthcare systems to share information with each other making it easier for doctors to get the information they need to make informed decisions about their patients’ care. This proves especially beneficial to parents and patients when they need to transition care or seek a second opinion at Texas Children’s.
- Telemedicine. Using telecommunications technology to provide medical care from a distance has made it possible for patients to receive care even if they live in rural areas or have difficulty getting to a doctor’s office.
“When the system went live, I saw immediate value in the first clinic session. I had a patient with ear infections and because I could see all her Texas Children’s Pediatrics notes and medication history in Epic, I was able to make a surgical recommendation without requesting outside records,” said Dr. Carla Giannoni, chief medical information officer. “Today we use it for so much more, and Epic adds new modules and features every few months.”
Giannoni continued, “Epic has streamlined data collection so we can improve our operational processes, and that has resulted in added efficiency and convenience. I also absolutely love that I can get most of the Epic data I need on call through the mobile app, Haiku. I can see OR schedules, my team’s patient list as well as my schedule, and chat securely with the bedside nurse.”
Click here to view a video about the Epic anniversary. Congratulations to everyone at Texas Children’s for 15 years of Epic success.