 When Bristol Dunlap was born, she was perfectly healthy. But by the time she was three months old, she was failing to reach her milestones and began showing worrisome symptoms.
When Bristol Dunlap was born, she was perfectly healthy. But by the time she was three months old, she was failing to reach her milestones and began showing worrisome symptoms.
“She could not lift her head up or sit upright, her body was unusually floppy, and her left eye began turning inward even though her vision was fine,” said her mother Evonia Dunlap. “As my daughter grew older, she was slow to crawl, stand and walk, and had difficulties in chewing, swallowing and talking.”
Bristol was diagnosed with congenital hypotonia which explained her poor muscle tone throughout her body. While therapy helped her daughter sit, walk and talk, there was one thing Dunlap wanted to know: What caused Bristol to develop hypotonia?
After seeing many specialists and undergoing a battery of diagnostic tests with still no answer, the family’s five-year medical odyssey ended at the Jan and Dan Duncan Neurological Research Institute (NRI) at Texas Children’s, where they were referred to neurologist Dr. Hsiao-Tuan Chao and Dr. Michael Wangler, geneticist and assistant professor of Human and Molecular Genetics at Baylor College of Medicine.
Through the NIH-funded Undiagnosed Disease Network (UDN), which brings together experts from across the country to help solve mysterious medical conditions by searching for their genetic basis, Chao and Wangler learned of a 7-year-old boy who exhibited symptoms similar to Bristol’s and also carried a point mutation in the Early B-Cell Factor 3 (EBF3) gene.
After re-examining Bristol’s exome sequencing results, they found she, too, carried the same mutation that produces a defective EBF3 protein. Since this protein is a master regulator of hundreds of other genes, even the tiniest alteration in its function could potentially cause widespread damage to the nervous system and muscles.
A referral center for undiagnosed diseases
Like the Dunlaps, many patient families are referred to Texas Children’s because of our renowned expertise and specialization in the diagnosis of diseases that are rarely seen and often unrecognized. Besides bringing together experts in genetics, pediatrics and neurology at Texas Children’s and its academic partner, Baylor College of Medicine, the UDN unites clinicians and scientists from across the country to help solve the most difficult medical cases. It is one of seven UDN sites nationwide.
More than 50 percent of UDN patients exhibit neurological symptoms. Texas Children’s chief of Neurology Dr. Gary Clark is one of the co-leaders of the UDN program at Texas Children’s and Baylor, and works closely with Texas Children’s neurologist Dr. Lisa Emrick in solving these mysterious neurological disorders.
“When a patient is referred to our UDN site, their DNA sample is submitted for sequencing,” said Emrick. “We conduct phenotyping and provide our UDN and NRI partners with the clinical patient data they need to help identify variant genes that may be responsible for a patient’s disease. Before advanced technologies like sequencing, only a small percent of these cases could be diagnosed.”
In addition to state-of-the-art medical imaging, metabolomics, and genetic testing including genome sequencing and exome sequencing, clinicians and researchers in the UDN rely on the Model Organism Screening Center (MOSC), where genes are studied in fruit flies to help diagnose patients. The center is led by Dr. Hugo Bellen, professor of Molecular and Human Genetics and Neuroscience at Baylor; Dr. Shinya Yamamoto, NRI investigator and assistant professor at Baylor; and Wangler. This dynamic team uses fruit flies, Drosophila melanogaster, to study new disease candidate genes and variants. They also closely collaborate with researchers at the University of Oregon in generating zebrafish models to study origins of disease.
In the MOSC, researchers combine bioinformatics analysis and experimentation in these ideal organism models to determine whether a specific variant identified in the genome of the patients may be responsible for the disease. “Integration of human genomics and experiments in simple model organisms such as fruit flies and zebrafish greatly facilitates disease diagnosis and mechanistic studies,” said Bellen.
“An exciting technique we developed is a way to humanize a fly gene,” said Yamamoto. “By knocking out the homologous gene in the fly and replacing it with the human gene, we can test the specific variant found in the patient to see how well it performs.”
Since fruit flies share many similar genes with humans, they have become a powerful model organism for the study of genetics. To study human disease in fruits flies, scientists mutate, or disrupt, the same gene that is known or suspected to cause the disease, and then figure out why mutations with this gene leads to disease.
Through collaboration with the UDN, Texas Children’s and Baylor continue to make significant strides in helping to accelerate the diagnoses of previously undiagnosed and rare neurological conditions.
For the Dunlap family, this provides a source of encouragement.
“While the journey to find a cure for our daughter’s illness has just begun, we are happy to finally have some answers,” Evonia said. “We are thankful for the pioneering work being done by physicians and researchers at Texas Children’s.”
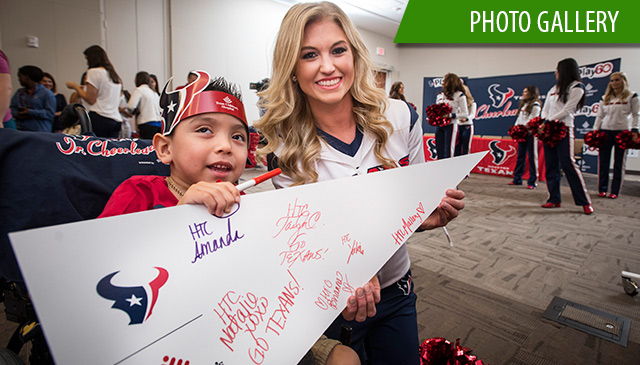 Patients got a special treat last week when the Houston Texans cheerleaders paid them a visit and hosted their third annual mini Jr. cheerleading camp at Texas Children’s Hospital.
Patients got a special treat last week when the Houston Texans cheerleaders paid them a visit and hosted their third annual mini Jr. cheerleading camp at Texas Children’s Hospital.
























 Texas Children’s work to develop a novel non-invasive device for pediatric ureteral stent removal after a urinary tract procedure, with Baylor College of Medicine, Rice University’s Oshman Engineering Design Kitchen (OEDK) and Department of Bioengineering, as well as local life sciences commercialization firm Fannin Innovation Studio, was recently funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health (NIH). The $225,000 Small Business Innovation Research (SBIR) grant will be used to conduct further development of an electromagnetic device for removal of ureteral stents in pediatric patients.
Texas Children’s work to develop a novel non-invasive device for pediatric ureteral stent removal after a urinary tract procedure, with Baylor College of Medicine, Rice University’s Oshman Engineering Design Kitchen (OEDK) and Department of Bioengineering, as well as local life sciences commercialization firm Fannin Innovation Studio, was recently funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health (NIH). The $225,000 Small Business Innovation Research (SBIR) grant will be used to conduct further development of an electromagnetic device for removal of ureteral stents in pediatric patients.













 “When we were at Texas Children’s for countless tests and procedures, wrestling for an elevator was the last thing we wanted to do,” wrote a Texas Children’s patient family. “Thank you to all of the staff and doctors who we saw taking the stairs. Seeing staff walk up or down a few flights of stairs was a kind gesture to free up space.”
“When we were at Texas Children’s for countless tests and procedures, wrestling for an elevator was the last thing we wanted to do,” wrote a Texas Children’s patient family. “Thank you to all of the staff and doctors who we saw taking the stairs. Seeing staff walk up or down a few flights of stairs was a kind gesture to free up space.” Orthopedic Surgeon Dr. Scott McKay was recently named a recipient of the 2017 Pediatric Orthopaedic Society of North America (POSNA) /Sociedad LatinoAmericana de Orthopedia Y Traumatologia Infantil (SLAOTI) Traveling Fellowship Award to South America.
Orthopedic Surgeon Dr. Scott McKay was recently named a recipient of the 2017 Pediatric Orthopaedic Society of North America (POSNA) /Sociedad LatinoAmericana de Orthopedia Y Traumatologia Infantil (SLAOTI) Traveling Fellowship Award to South America.