A year’s worth of planning and preparation came to fruition last month as Texas Children’s Hospital hosted the 24th Annual Society of Pediatric Liver Transplantation (SPLIT) Conference, bringing together experts from more than 40 national and international liver transplant centers.
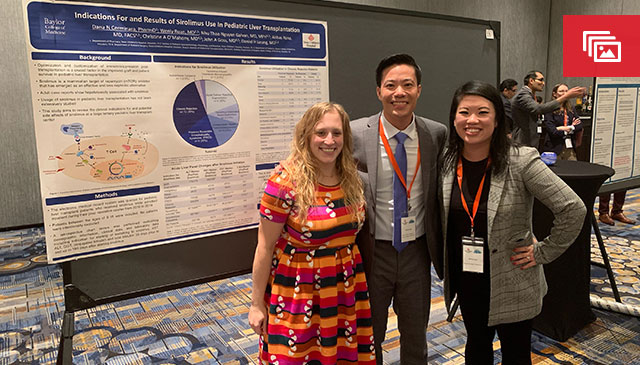
The two-day event, designed for health care professionals involved in the care of pediatric liver transplant patients, featured speaker presentations, panel discussions, and case and poster presentations. Major discussion session topics included:
- Unique Transplant Considerations
- A Village Approach to Liver Intensive Care
- Surgical and Interventional Considerations
- The Many Faces of Rejection
- Advocacy
Texas Children’s multidisciplinary approach to liver transplant care was on display throughout. Of the 36 presenters who spoke, 15 were from Texas Children’s and academic affiliate Baylor College of Medicine. This year’s SPLIT meeting also boasted the best attendance ever, with 236 attendees, which included physicians, surgeons, advanced practice providers, trainees, data and transplant coordinators, dietitians and social workers.
The event was spearheaded by Dr. Daniel Leung, Texas Children’s Director of Pediatric Hepatology and Liver Transplant Medicine, and the event’s Continuing Medical Education (CME) Activity Director; and Melissa Nugent, education coordinator for Transplant Services, who was the event organizer and the meeting’s Nurse Planner for Continuing Nursing Education. Thanks in large part to the planning committee, the conference was such a success that it won Texas Children’s award for Best CME Course.
The planning committed included:
- Dr. John Goss, Medical Director of Transplant Services
- Diesa Samp, Director of Transplant Services
- Julie Economides, RN, SPLIT data coordinator at Texas Children’s
“It was an honor to be selected to host this year’s SPLIT Conference,” said Leung. “We not only showcased the breadth of our subspecialty expertise – including ICU, infectious diseases, immunology, interventional radiology, transfusion medicine, nephrology and others – all dedicated to pre- and post-lever transplant care at Texas Children’s, but we also continue to lead the country by example in how we collaborate and learn from one another. I am truly grateful for our special team of surgeons, hepatologists, coordinators, nurses, pharmacists, dietitians and social workers. It really does take a village.”
About SPLIT
The Society of Pediatric Liver Transplantation is a unique multidisciplinary, multicenter consortium focused on optimizing outcomes pediatric liver transplantation through research, advocacy, and dissemination of best practice in this field. SPLIT is the only such academic body dedicated to pediatric liver transplantation.
About Transplant Services at Texas Children’s
Transplant Services at Texas Children’s was the nation’s largest pediatric transplant program in 2018, performing a remarkable 107 solid organ transplants including the highest volumes of pediatric liver, lung and kidney transplants.
Transplant Services provides a comprehensive, multidisciplinary approach to care through all aspects of the transplant process, from initial referral to hospitalization and outpatient management. Our team of experts includes physicians and surgical advanced practice providers, transplant coordinators, pediatric ventricular assist device coordinators, perfusionists, child life specialists, dietitians, social workers, financial counselors, pharmacists, inpatient and outpatient nursing and support staff, Perioperative Services, physical and occupational therapists, Radiology, Pathology, our LifeGift partners, and many others.
Our depth of skill and service enables us to offer world-class care for patients, from newborns to young adults, in need of heart, kidney, liver and lung transplants. That expertise has allowed us to successfully treat some cases that other national and international programs might consider untreatable.
Learn more about Transplant Services at Texas Children’s Hospital.